Table of Contents
Multifocal atrial tachycardia (MAT) is a rare, poorly understood, and commonly misdiagnosed dysrhythmia. The overall prevalence of MAT is <0.4%.
Causes of Multifocal Atrial Tachycardia (MAT)
When present, it is usually seen in acutely ill patients, such as those with:
- hypoxia
- hypercarbia
- hypokalemia
- hypomagnesemia
- hyperadrenergic states
- acute exacerbations of chronic disease
In fact, it is felt that MAT reflects the severity of the underlying disease process.
The most common misdiagnoses of MAT are atrial fibrillation (Afib) and sinus tachycardia. Since the treatment of each of these dysrhythmias is different, it is imperative for the emergency provider to correctly diagnose MAT.
Differentiating between Multifocal Atrial Tachycardia and Atrial Fibrillation
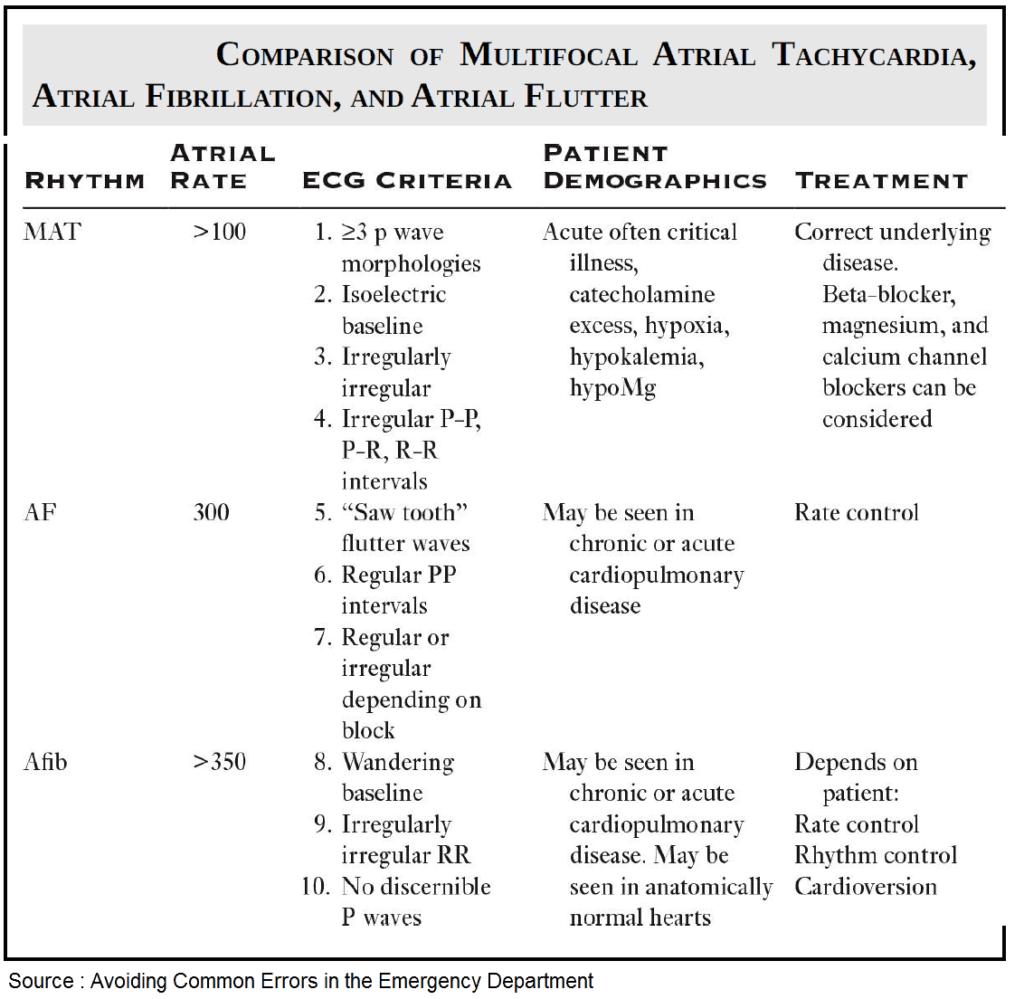
Differentiating between MAT and Afib can be a challenge for providers. Both dysrhythmias are irregularly irregular, can cause rapid ventricular rates, and more commonly occur in elderly patients with existing cardiopulmonary disease. In addition, MAT can occasionally be associated with other atrial dysrhythmias, including Afib and atrial flutter (AF).
The most commonly accepted diagnostic criteria for MAT are:
- the presence of at least three morphologically distinct P waves in a single electrocardiogram (ECG) lead
- an atrial rate greater than or equal to 100 beats per minute
- an isoelectric baseline between P waves
P waves in MAT are well formed and discrete, compared to Afib where P waves are characterized as continuous, undulating, and changing.
Additional features include the absence of a dominant pacemaker and irregularly irregular P-P, P-R, and R-R intervals. This Table lists key features of MAT, Afib, and AF.
Treatment of Multifocal Atrial Tachycardia (MAT)
Treatment of MAT is aimed at the underlying diseases process that caused the dysrhythmia. In contrast to Afib and AF, MAT does not usually respond to cardioversion or pharmacologic therapy.
Ensuring adequate oxygenation and ventilation, repletion of potassium and magnesium, and reduction of any exogenous adrenergic stimulation should be prioritized. In addition, it is important to review the patient’s medications and remove any potential medications that may precipitate MAT.
Remove any potential medications that may precipitate MAT
As many patients with MAT have severe pulmonary disease, it is possible that some are receiving chronic therapy with a methylxanthine medication, namely, theophylline. Theophylline use and toxicity have been associated with MAT, and theophylline should be discontinued in the setting of MAT.
Experts also believe that beta-agonist medications used to treat bronchospasm may propagate MAT. If possible, beta-agonist administration should be reduced if MAT develops, though this may be challenging in the patient with acute exacerbations of chronic obstructive pulmonary disease (COPD).
Beta-blockers, calcium channel blockers, and magnesium sulfate
Beta-blockers, calcium channel blockers, and magnesium sulfate have been investigated in the treatment of MAT and have shown improved ventricular rates, at the expense a reduction in blood pressure.
- To date, the majority of evidence has been on the use of beta-blockers (i.e., metoprolol, esmolol) for the treatment of MAT. However, the administration of beta-blockers remains controversial in the setting of patients with COPD.
- Verapamil has been evaluated in the treatment of MAT. While it does reduce heart rate, it can cause a profound and sustained drop in blood pressure and should be avoided in critically ill patients.
- Magnesium has an acceptable adverse effect profile and has been shown to have reasonable efficacy in heart rate reduction and conversion to sinus rhythm.
In general, medical therapy to reduce heart rate should be attempted after optimization and treatment of the underlying disorder. MAT rarely causes hypotension and shock. If either is present in a critically ill patient, a search for another etiology should be performed.
Read More about Management of Atrial Fibrillation (AF) with Rapid Ventricular Response (RVR)
Key Points
- The most common misdiagnoses for MAT are Afib and sinus tachycardia.
- MAT requires the presence of at least three morphologically different P waves in a single ECG lead.
- Treatment of MAT is aimed at the underlying disease process.
- Theophylline is associated with MAT. If possible, discontinue this medication.
- MAT rarely causes shock. If shock is present, search for another etiology.
Suggested Readings
- Borzak S, McCord J. Multifocal atrial tachycardia. Chest. 1998;113:203. https://pubmed.ncbi.nlm.nih.gov/9440591/
- Hill G, Owens S. Esmolol in the treatment of multifocal atrial tachycardia. Chest. 1992;101:1726. https://www.sciencedirect.com/science/article/abs/pii/S0012369216384380
- Kastor J. Multifocal atrial tachycardia. N Engl J Med. 1990;322:1713–1717. https://www.nejm.org/doi/full/10.1056/NEJM199006143222405
- Schwartz M, Rodman D, Lowestein S. Recognition and treatment of multifocal atrial tachycardia: A critical review. J Emerg Med. 1994;12(3):353–360. https://pubmed.ncbi.nlm.nih.gov/8040593/
- Ueng KC, Lee SH, Wu DJ, et al. Radiofrequency catheter modification of atrioventricular junction in patients with COPD and medically refractory atrial tachycardia. Chest. 2000;117:52. https://www.sciencedirect.com/science/article/abs/pii/S0012369215309296

![Read more about the article Left Ventricular Hypertrophy (LVH): How to Recognize it on ECG [With Examples]](https://manualofmedicine.com/wp-content/uploads/2025/12/Summary-of-the-various-diagnostic-ECG-criteria-for-left-ventricular-hypertrophy-LVH.png)