Table of Contents
In the hectic environment of the emergency department, rapid diagnosis and emergent management of life-threatening conditions must occur.
In the patient with acute chest pain and an electrocardiogram (ECG) concerning for an ST-segment elevation myocardial infarction (STEMI), the diagnosis and treatment seem straightforward. National guidelines recommend emergent reperfusion with percutaneous coronary intervention (PCI) or fibrinolytic therapy.
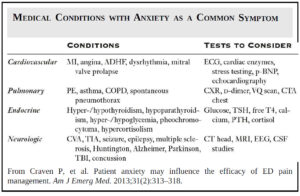
Unfortunately, the potential for patient harm is high when an acute aortic dissection (AD) causes an acute coronary syndrome (ACS) and produces ischemic ECG changes.
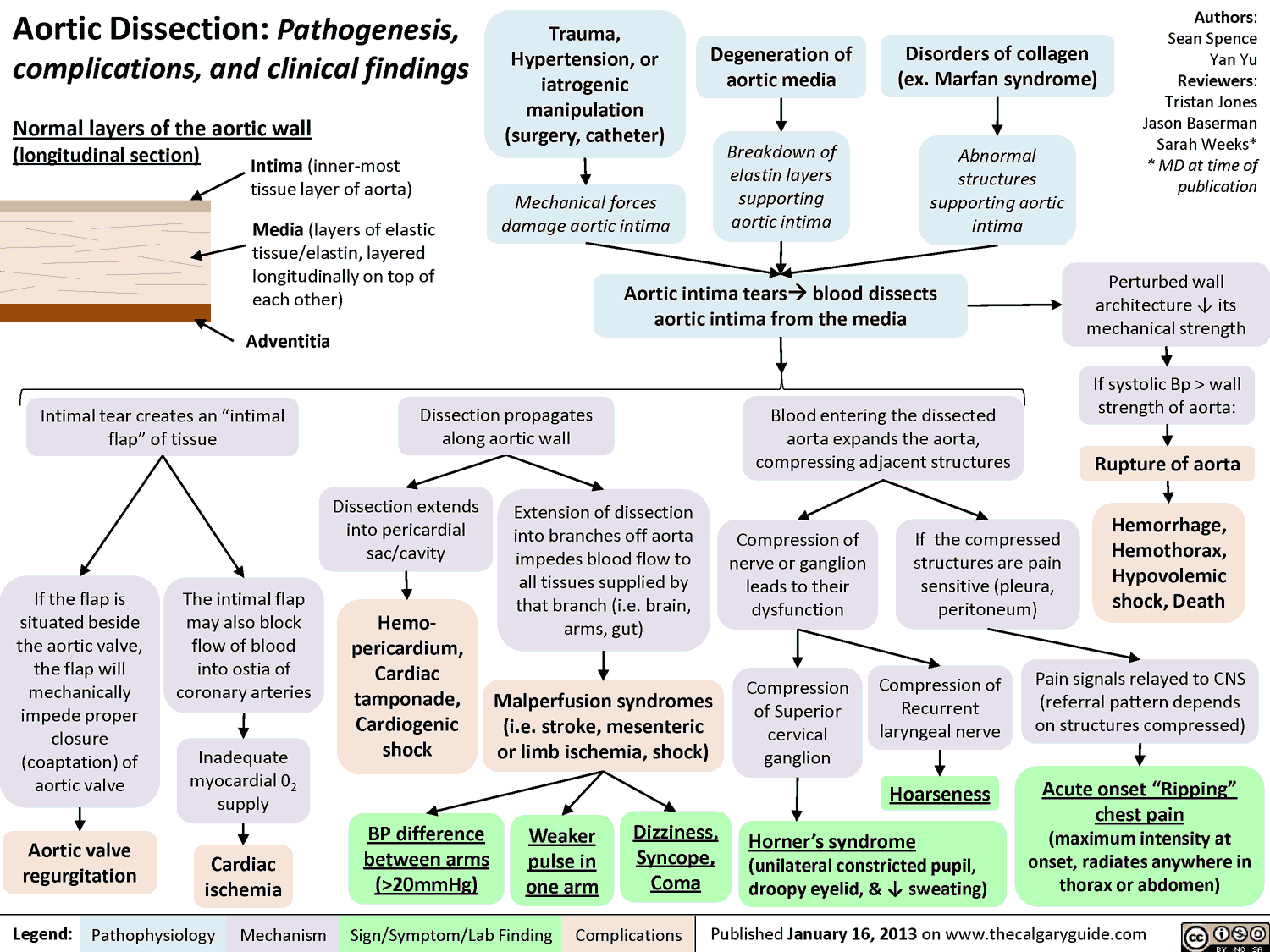
Pathophysiology and Pathogenesis
In Aortic Dissection, a defect in the aortic intima allows entry of blood into the tunica media. A false lumen develops and can propagate in an anterograde or retrograde direction.
Aortic Dissections that involve the ascending aorta (Stanford type A) can cause coronary insufficiency by several mechanisms. These include:
- a circumferential intimal defect of the ascending aorta that drapes over the coronary ostia
- an intimal defect involving the coronary ostia itself
- propagation of the false lumen into the coronary vessel that compresses the true lumen
- circumferential intimal detachment within the coronary artery causing intussusception of the inner vessel wall.
The right coronary artery is the most common vessel affected by these pathologic mechanisms. As a result, an inferior STEMI is the most common ACS presentation in patients with Aortic Dissection.
Notwithstanding, case reports exist of acute Aortic Dissection with coincident STEMI without the dissection directly involving the coronary vessel (e.g., STEMI with Stanford type B).
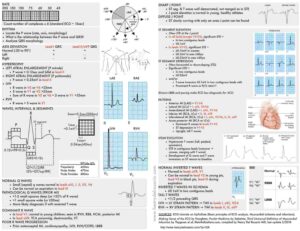
ECG Changes in Aortic Dissection
Approximately 70% of patients with acute Aortic Dissection will have an ECG abnormality. These can include:
- nonspecific ST-segment or T-wave changes
- left ventricular hypertrophy (LVH)
- atrial dysrhythmias
Diffuse ST-segment elevation, with or without PR segment depression, and electrical alternans should raise suspicion for pericardial effusion caused by aortic rupture into the pericardial space.
While the rate of Aortic Dissection in patients with STEMI is very low (0.1% to 0.2%), the rate of STEMI is 5% in patients with an Aortic Dissection. This rate rises to 8% when considering only those patients with a type A dissection.
Consider the diagnosis of Aortic Dissection, especially in patients with an inferior STEMI. Additional history and physical examination findings may prevent catastrophic results from antiplatelet, anticoagulant, or fibrinolytic therapy.
Importantly, an anterior STEMI is rarely, if ever, associated with an acute AD.
How should the clinician approach the patient with acute chest pain, ischemic ECG findings, and risk factors for an acute Aortic Dissection?
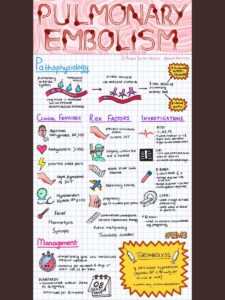
A presentation in which acute Aortic Dissection is strongly suggested and an inferior or posterior STEMI is noted on ECG should prompt rapid evaluation of the thoracic aortic.
Fibrinolytic therapy should be withheld until Aortic Dissection can be excluded. Confirmation or exclusion of AD can be rapidly accomplished with computed tomography of the chest and abdomen.
Emergent PCI can also establish the diagnosis in select cases. When the clinical presentation is concerning for an acute AD and nondiagnostic ECG abnormalities are seen, a similar diagnostic-therapeutic approach is warranted.
Key Points
- Up to 70% of patients with acute Aortic Dissection will have an ECG abnormality.
- Up to 8% of type A dissections can be complicated by STEMI.
- The right coronary artery is the most common artery involved in cases of Aortic Dissection.
- An anterior STEMI is rarely associated with an acute Aortic Dissection.
- Do not administer fibrinolytic therapy to STEMI patients in whom there is suspicion of an acute Aortic Dissection.