Table of Contents
General Approach and Resuscitation
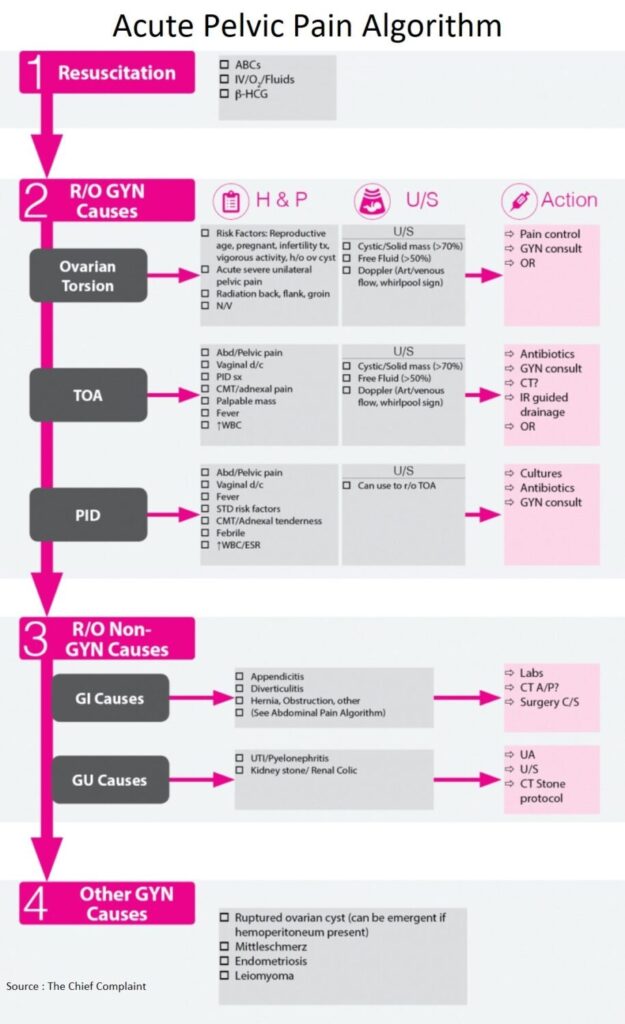
- The approach to the woman with pelvic pain is to start with the initial resuscitation and β-HCG
- Then the focus should be on emergent gynecologic disease, such as ovarian torsion and PID / TOA (Tuboovarian Abscess)
- Then expand the differential to think about non-gynecologic causes from Genitourinary or Gastrointestinal origin, most commonly Appendicitis
- If that work-up is negative, consider treating empirically for PID, and think about other causes of pelvic pain
Emergent Gynaecological Causes
1. Ovarian Torsion
General
- Definitive diagnosis of ovarian torsion is based on surgical findings
- Difficult diagnosis → correct pre-operative diagnosis made in only 38% of cases (J Reprod Med 2000;45:831)
Clinical Presentation
- Risk Factors: Reproductive age, pregnant, infertility therapy, vigorous activity
- Acute severe unilateral pelvic pain
- Radiation to back, flank, groin
- Nausea / Vomiting
Ultrasound
- Cyst/Mass (Clin Exp Obstet Gynecol 2004;31:34)
- Found in >94% of torsion cases
- Most commonly, mass is greater than 5cm
- Normal ovaries (absence of cyst/mass) does not completely rule-out torsion
- Normal ovaries found in 6% of adult cases and over 50% of children under age 15 (Arch Pediatr Adolesc Med 2005;159:532-535)
- Doppler blood flow (J Clin Ultrasound. 2009;37(8):436)
- Predictive of non-viability of the ovary
- Blood flow preserved in early/incomplete torsion or torsion/detorsion
- Whirlpool sign (J Ultrasound Med 2004;23:1643–1649)
- Sonographic appearance of twisted vascular pedicle
- Earliest and most definitive sign for torsion
- Caution
- Ovaries have dual blood supply, therefore, the presence of normal flow does not exclude torsion
- If high clinical suspicion (persistent pain) → may need laparoscopy despite negative ultrasound
Treatment:
- Pain control
- Gyn consult for surgical evaluation
2. Tuboovarian Abscess (TOA)
General: Tuboovarian Abscess
- Definition: Inflammatory mass in fallopian tube/ovary/pelvic organs, found most commonly in reproductive age women and typically results from upper genital tract infection
- Etiology:
- PID (most common)
- pelvic surgery
- intra-abdominal process
- Microbiology: same as PID, polymicrobial, anaerobes
Clinical Presentation
- Abdominal/Pelvic pain
- PID symptoms, Vaginal discharge
- CMT / adnexal pain
- Palpable mass
- Fever, High WBC
Diagnosis
- Consider in any woman suspected of PID
- Ultrasound:
- Homogeneous, cystic mass with air/fluid levels and septations
- Utility (Journal Emerg Med 2011;40:170)
- Newer studies show sensitivities that range from 56% to 93%, with a specificity of 86% to 98%
- Low sensitivity of Ultrasound → cannot rule out Tuboovarian Abscess, especially in the high risk patient
- If Ultrasound negative → may need CT to continue evaluation for Tuboovarian Abscess
- Helps differentiate TOA (Tuboovarian Abscess) vs TOC (tubo-ovarian complex) → perfused inflammatory living tissue without abscess wall, amenable to medical therapy
Treatment
- Medical: Trial of medical therapy (antibiotics) vs
- IR guided drainage vs
- Surgery: operative drainage
3. Pelvic Inflammatory Disease (PID)
General
- Represents a spectrum of disease from endometritis to fatal intra-abdominal sepsis
Clinical Presentation
- Abdominal / Pelvic pain
- Vaginal discharge
- Fever
- STD risk factors
- CMT/adnexal tenderness
- High WBC / ESR
Diagnosis
- US
- Rule-out TOA
- May be diagnostic of PID
- CDC has issued a minimum set of criteria for treatment of PID for women with abdominal pain and at least one of the criteria (See Table) (MMWR Recomm Rep 2010;59:1-110)
Criteria for Treatment of PID
□ CMT or uterine/adnexal tenderness
□ Oral Temp > 101F
□ Leukocytosis/left shift
□ Abnormal cervical/vaginal discharge
□ Vaginal secretions with WBC on saline microscopy
□ Elevated ESR
□ Elevated CRP
Treatment
- Outpatient treatment
- If stable, well appearing, tolerating po, pain controlled → can be discharged on po antibiotics
- Antibiotics (see most recent CDC guidelines)
- Inpatient treatment
- If patient meets criteria for hospitalization → start IV antibiotics, admit
Criteria for Hospitalization
□ Surgical emergencies (e.g., appendicitis) cannot be excluded
□ Pregnant
□ Does not respond clinically to oral antimicrobial therapy
□ Unable to follow or tolerate an outpatient oral regimen;
□ Severe illness, nausea and vomiting, or high fever; and
□ Tubo-ovarian abscess
Rule Out Non Gynaecological Causes
- See Abdominal Pain algorithms for more detailed explanation of GI and GU causes of abdominal pain
- Consider Appendicitis vs Diverticulitis (possible CT AP)
- Consider UTI (Check Urinalysis)
- Consider renal colic (UA, US, CT Stone?)
Other Gynaecological Causes
OVARIAN CYST RUPTURE
- Sudden onset, unilateral abdominal pain, +/- vaginal bleeding, +/- peritoneal signs (blood irritating peritoneum)
- Uncomplicated (follicular or corpus luteum cyst) → follow expectantly for enlarging hemoperitoneum
- Complicated: may need surgical management, blood transfusion
MITTELSCHMERZ
- Mid-cycle pain from rupturing of follicle during ovulation
References
- Torsion of the uterine adnexa. Pathologic correlations and current management trends. https://pubmed.ncbi.nlm.nih.gov/11077633/
- Uterine adnexal torsion: pathologic and gray-scale ultrasonographic findings. https://pubmed.ncbi.nlm.nih.gov/14998184/
- Urgency of evaluation and outcome of acute ovarian torsion in pediatric patients. https://pubmed.ncbi.nlm.nih.gov/15939851/
- Doppler studies of the ovarian venous blood flow in the diagnosis of adnexal torsion. https://pubmed.ncbi.nlm.nih.gov/19670236/
- Sonographic whirlpool sign in ovarian torsion. https://pubmed.ncbi.nlm.nih.gov/15557307/
- Sensitivity of Ultrasound for the Diagnosis of Tubo-Ovarian Abscess: A Case Report and Literature Review. https://www.sciencedirect.com/science/article/abs/pii/S0736467910001812
- Sexually transmitted diseases treatment guidelines, 2010. https://stacks.cdc.gov/view/cdc/6119