Table of Contents
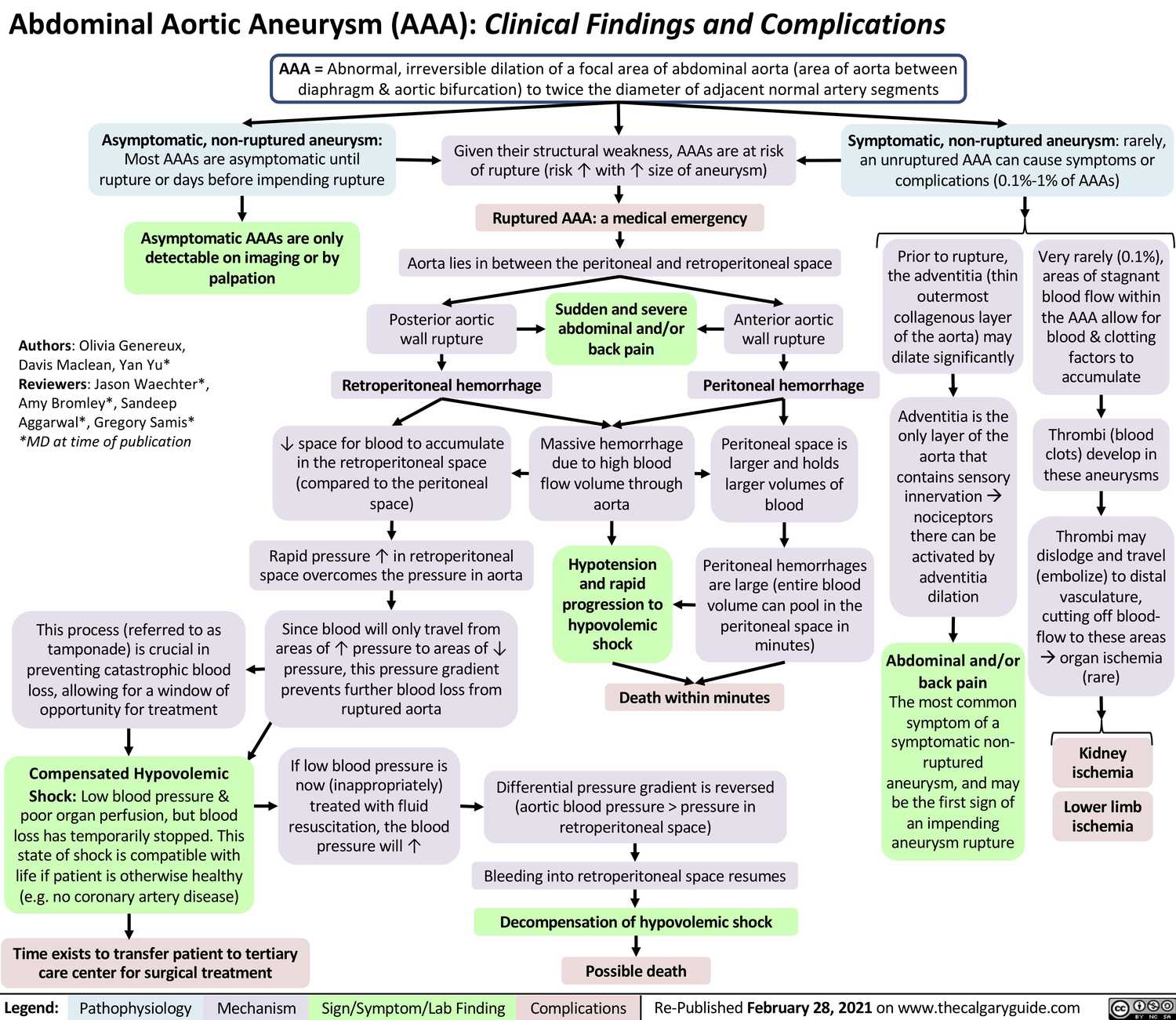
Abdominal Aortic Aneurysm (AAA)
Epidemiology
- 4-6 : 1 Male : Female ratio
- 4-8% if age > 65
- Most infrarenal
Etiology
- Usually due to atherosclerotic disease
- Risk factors:
- smoking
- male sex
- age
- pre-existing atherosclerosis
- obesity
- Hyperlipidemia
- HTN (Hypertension)
- Family History
Screening / Surveillance
- ACC/AHA: One-time abdoimnal ultrasound in all men older 60 years with or without Family History of AAA (IIC) and all men > 65 that have ever smoked (IA)
- USPSTF: One-time abdominal ultrasound for men age 65-75 who have ever smoked (Grade B) and selective screening for male who never smoked 65-75 (Grade C). Screening for women not recommended.
- Surveillance:
- 3-3.4 cm: U/S q3y
- 3.5-4.4 cm: U/S or CT q12mo
- 4.5-5.4 cm: U/S or CT q6mo
Imaging Modalities
- Abdominal Ultrasound: screening and surveillance of infrarenal AAAs. High Se/Sp (>90%), operator-dependent
- CT w/ contrast: high Se/Sp, better than U/S for suprarenal AAAs
- MRI/MRA: good Se/Sp, preferred for aortic root imaging and for imaging tortuous aortas
- CXR: “enlarged aorta” nonspecific (tortuous aorta vs. aneurysm)
- TTE (transthoracic echocardiogram): useful for root and proximal thoracic aorta; TEE: will visualize entire thoracic aorta but rarely used.
Treatment
Medical:
- Smoking cessation (slows AAA growth by up to 25%)
- Reduce Blood Pressure in accordance with ACC/AHA standards
- Meds:
- Statins (reduce all-cause mortality in patients post surgery)
- Beta Blockers (may slow expansion; IA for perioperative use)
- ACEi (controversial; may prevent rupture but may speed growth)
- Low dose ASA (may slow growth)
- Antibiotics (e.g., roxithromycin may reduce expansion rate ,not mortality)
Surgical:
- Men: > 5.5 cm OR growing at >0.5 cm/year OR symptomatic Women: > 4.5-5cm (controversial)
- Open repair (~4-6% 30 day mortality) vs. EVAR (only~50% suitable, c/b endoleaks [continued blood flow intoaneurysmal cavity, ~1% 30 day mortality]).
Complications
- Rupture: Devastating mortality. AAA annual rupture rates are 4%, 7%, 20% at 5, 6, and 7cm, respectively.
- Risk factors for Rupture:
- size,
- rate of expansion,
- female gender
- Symptoms of AAA Rupture: Triad of:
- abdominal / back pain
- pulsatile abdominal mass
- hypotension
- Immediate surgery (don’t image)
- Risk factors for Rupture:
- Dissection: pain (chest/abdomen/back), occlusion of aortic vessels, thromboembolism
- Post-repair:
- EVAR: endoleak, graft failure, thrombosis.
- Open: MI, embolization, AKI, ischemic colitis
Thoracic Aortic Aneurysm (TAA)
Epidemiology
- 1.7 : 1 Male : Female ratio
- Mostly age of 50-70
- 50% Ascending Aorta, 40% Descending Aorta, 10% Aortic Arch
Etiology
- Atherosclerotic: Majority of cases. Mostly in Descending Aorta.
- Risk factors:
- Smoking,
- Hyperlipidemia,
- HTN (Hypertension)
- Risk factors:
- Structural/genetic: Mostly in root and ascending aorta.
- Causes:
- Connective tissue disease (Marfan, Ehlers-Danlos, Loeys-Dietz)
- Turner syndrome
- Bicuspid Aortic Valve
- Trauma
- Causes:
- Infectious:
- tertiary syphilis
- mycotic aneurysm (mostcommon organisms: Staphylococcus spp., Salmonella spp.)
- Inflammatory:
- GCA (Giant cell arteritis): ~10% have TAA
- Takayasu arteritis
- Rheumatoid arthritis
- Psoriasis
- Behcet’s
- Wegener’s Granulomatosis
Screening / Surveillance
- General population: Not recommended
- Indications:
- At time of diagnosing Marfan (IC), Turner (IC) ,Loeys-Dietz, Takayasu arteritis or (Giant cell arteritis).
- 1st degree relatives of patients with TAA, dissection, bicuspid valve (IB/IC).
- Surveillance:
- If aneurysm only, then same as AAA.
- If also with dissection, image at 1, 3, 6, & 12 months then annually.
- Image entire aorta (CT/MRI) if multiple aneurysms (~25% TAA will have AAA; ~25% AAA will have TAA).
Imaging Modalities
- Abdominal Ultrasound: screening and surveillance of infrarenal AAAs. High Se/Sp (>90%), operator-dependent
- CT w/ contrast: high Se/Sp, better than U/S for suprarenal AAAs
- MRI/MRA: good Se/Sp, preferred for aortic root imaging and for imaging tortuous aortas
- CXR: “enlarged aorta” nonspecific (tortuous aorta vs. aneurysm)
- TTE (transthoracic echocardiogram): useful for root and proximal thoracic aorta; TEE: will visualize entire thoracic aorta but rarely used.
Treatment
Medical:
- Reduce BP (<140/90 or <130/80 if DM or CKD; littl eactual evidence, IB)
- Smoking cessation; avoid straining
- Stress test used to guide BP management (follow SBP response to stress)
- Meds:
- Beta Blockers proven to decrease TAA growth in Marfan
- ARBs slow aortic root aneurysm expansion in Marfan patients, likely via TGF-B inhibition (NEJM 2008;358:2787)
- Statins if LDL<70, some evidence
Surgical:
- Root / ascending TAAs: usually concomitant aortic valve replacement
- Arch / descending TAAs: mostly open graft, (EVAR). Ischemic brain/spine injury most worrisomecomplication.
Complications
- Rupture: Devastating mortality. AAA annual rupture rates are 4%, 7%, 20% at 5, 6, and 7cm, respectively.
- Risk factors for Rupture:
- size,
- rate of expansion,
- female gender
- Symptoms of TAA Rupture: Triad of:
- abdominal / back pain
- pulsatile abdominal mass
- hypotension
- immediate surgery (don’t image)
- Risk factors for Rupture:
- Dissection: pain (chest/abdomen/back), occlusion of aortic vessels, thromboembolism
- Post-repair:
- EVAR: endoleak, graft failure, thrombosis.
- Open: MI, embolization, AKI, ischemic colitis