Table of Contents
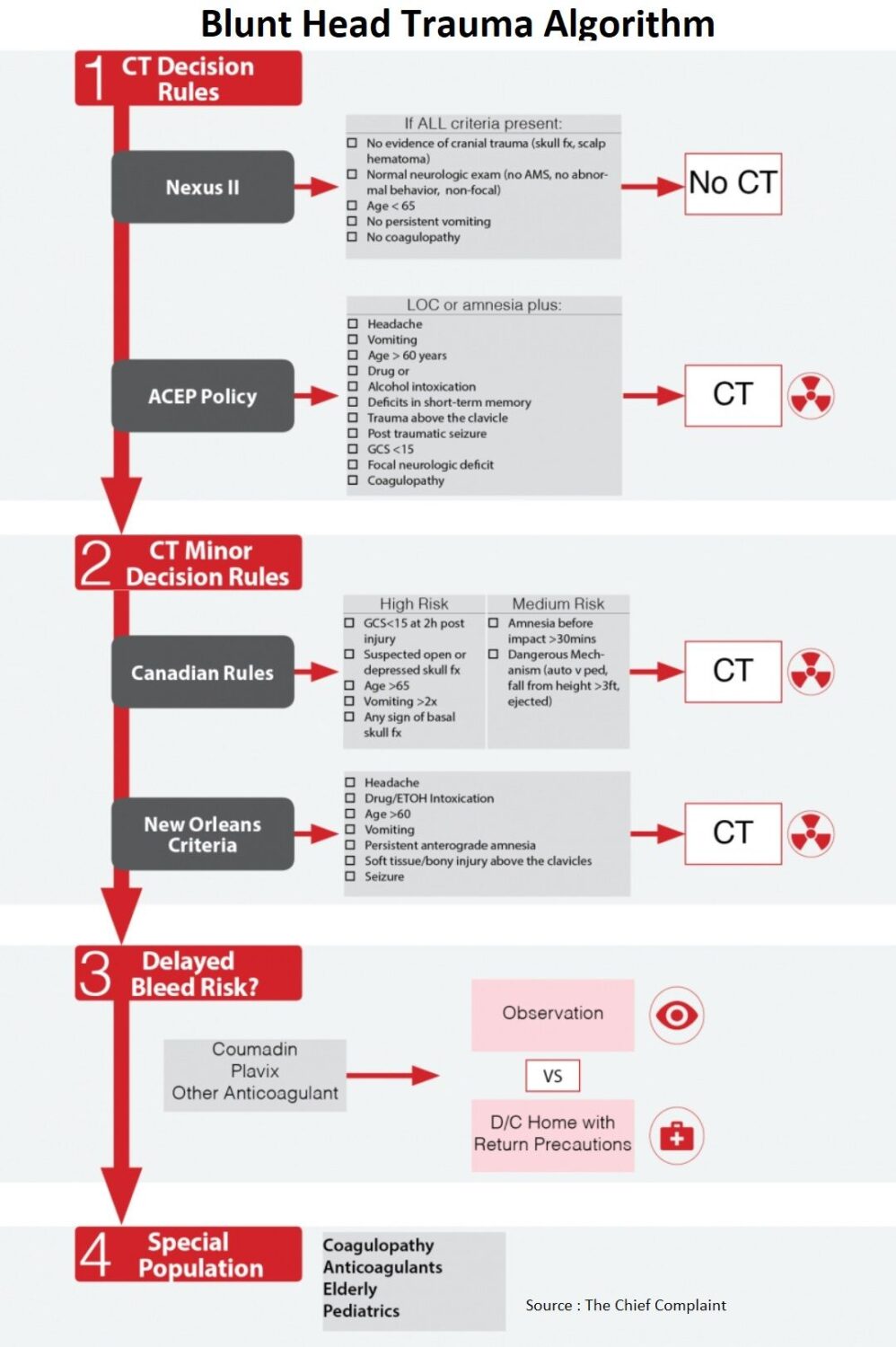
Head CT Rules
Nexus II (J Trauma 2005;59:954–959)
- Criteria highly associated with intra-cranial injury:
- Evidence of significant skull fracture
- Scalp hematoma
- Neurologic deficit
- Altered level of alertness
- Abnormal behavior
- Coagulopathy
- Persistent vomiting
- Age 65 years or more
- Evidence:
- Clinically significant injuries: Sens 98.3; NPV 99.1%; Specificty-13.7%
- Expected miss rate: approximately 1.7% of cases with “clinically important” intracranial injuries
- Use: Identify patients that are low risk that don’t need further imaging, not useful in deciding who does need imaging
ACEP Clinical Policy (Ann Emerg Med. 2008;52:714-748)
- A head CT is indicated in head trauma patients with loss of consciousness or posttraumatic amnesia only if one or more of the following is present (Level A Recommendation):
- Headache
- Vomiting
- Age greater than 60 years
- Drug or alcohol intoxication
- Deficits in short-term memory
- Physical evidence of trauma above the clavicle
- Posttraumatic seizure
- GCS score less than 15
- Focal neurologic deficit
- Coagulopathy
- A head CT should be considered in head trauma patients with no LOC or posttraumatic amnesia if there is (Level B Recommendation):
- Focal neurologic deficit
- Vomiting, severe headache
- Age 65 years or greater
- Physical signs of a basilar skull fracture
- GCS score less than 15
- Coagulopathy
- Dangerous mechanism of injury*
- * Dangerous mechanism of injury includes ejection from a motor vehicle, a pedestrian struck, and a fall from a height of more than 3 feet or 5 stairs.
Other Head CT Rules (For Your Consideration)
Canadian (Lancet. 2001;357:1391-6)
- Clinically important brain injury Sens 98%, Specificity 50%
- Neurosurgical intervention Sens 100%, Specificity 68%
- Complicated algorithm, extensive inclusion criteria for study, difficult to use in practice
- Inclusion Criteria:
- LOC, amnesia, disorientation
- GCS >13
- Age >16
- No penetrating skull injury
- Not pregnant
- No focal deficit
- No coagulopathy
- No seizure
- No unstable vital signs
New Orleans (NEJM 2000;343(2):100)
- Too sensitive and non-specific (Sens 100%, Spec 24%)
- Limitations: limited applicability, wide confidence intervals, has not been validated, used any injury as outcome measure
- Imaging obtained for any patient with trauma above clavicles → decreases specificity
- Inclusion criteria
- Age >3yo
- +LOC
- Normal neuro exam
- GCS 15
Delayed Bleed Risk
Delayed bleed Evidence
- Immediate intracranial hemorrhage (Blunt Head Trauma + Anticoagulation)
- ICH is a real entity with occurrence of 10-15%
- Any patient with head trauma on warfarin or clopidogrel should get an initial Head CT scan
- Delayed intracranial hemorrhage (Blunt Head Trauma + Anticoagulation + CT neg)
- Delayed ICH is also a real entity
- Increased risk in elderly and INR >3
- Observation option: admit for 24 h observation and repeat CT?
- Discharge option: Low risk, reliable, family present and able to return for any subtle changes
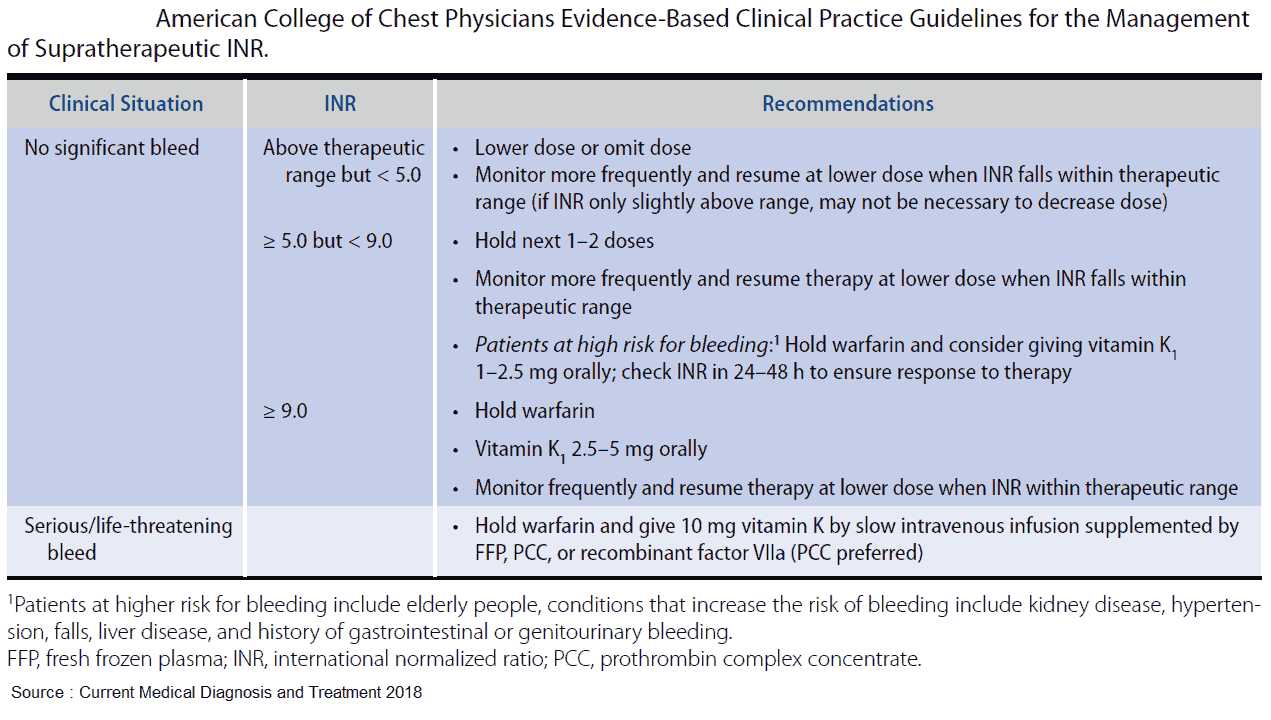
INR Reversal
- FFP
- 15cc/kg begins working immediately
- Use if PCC not readily available
- Vitamin K
- INR > 10 → Vit K 2.5-5mg po
- Serious/Life threat bleed → 10mg IV over 30 min (prevents anaphylactoid reaction)
- Begins working at 4 hours, full effect at 24h
- Prothrombin Complex Concentrate (PCC, KCentra)
- Concentrated clotting factors affected by warfarin (factors II, VII, IX and X)
- Use: Any serious or life threatening bleed
- VS FFP: PCC has a smaller volume, higher concentration of factors, complete reversal, only one dose in 24h, no need for thawing
- PCC in the ER (Circulation. 2013;128:360)
- Lower Adverse event: FFP:19.5% patients and PCC: 9.7%
- PCC: faster time to reversal (5.7 to 11.8 hours) and about half as much blood transfused vs FFP
- No increase in blood clots/DVT/PE
| Pre Treatment INR | 2-4 | 4-6 | >6 |
| Dose of 4-PCC (U/kg) | 25 | 35 | 50 |
| Max Dose | 2500 | 3500 | 500 |
Read More About :
- Threatening Hemorrhage in the Patient Taking an Oral Anticoagulant Medication
- Reversal of Anticoagulant Therapy
Journal Club: Delayed Bleed Risk in BHT
Study 1 (Ann Emerg Med 2012;59(6):460)
- Immediate bleed higher with Clopidogrel:
- Clopidogrel 12.0%; vs Warfarin 5.1%; (relative risk 2.3)
- Delayed bleed only seen in Warfarin:
- Warfarin: 0.6% (4 of 687 pts) vs Clopidogrel: 0% (0 of 243pts)
- Patients with delayed bleeds on warfarin, all had a GCS of 15 and 50% died
Study 2 (Ann Emerg Med 2012;59:451)
- Prospective case series of patients with BHT on warfarin with normal initial CT
- 6% (5 pts) delayed bleed risk on repeat CT, only 1 had neuro changes
- 2% returned with bleeds even after the 24 hour observation period and two negative head CTs.
- The relative risk of delayed hemorrhage with an initial INR > 3.0 was 14 (RR = 14)
Special Populations
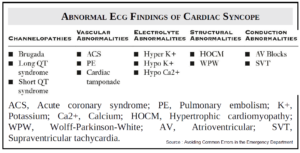
- Loss of Consciousness
- Increased prevalence of injury but not present as an independent predictor when control for other variables
- Do not use as indicator for CT imaging
- Seizure
- Not associated with increased prevalence of injury
- Infrequently seen, difficult to assess if truly had a seizure vs syncope
- Intoxication
- Decreased prevalence of injury → likely because of over-imaging intoxicated patients
- Need to improve risk stratification
- Elderly
- High prevalence of occult head injury and delayed bleeds
- Does not require high mechanism of injury (usually GLF) and increased use of anticoagulants
- Have low threshold for CT, admission, correction of coagulopathy and re-imaging
- Normal CT
- Altered Mental Status on presentation → concern for Diffuse Axonal Injury (DAI)
- Coagulopathy → Observation for delayed intracranial hemorrhage vs Discharge home with strict return precautions
Concussion
Diagnosis
- Symptoms: somatic (e.g. headache), cognitive (e.g. feeling like in a fog) and/or emotional symptoms (e.g. lability)
- Physical signs (e.g. loss of consciousness (LOC), amnesia)
- Behavioral changes (e.g. irritability)
- Cognitive impairment (e.g. slowed reaction times)
- Sleep disturbance (e.g. insomnia)
On-field evaluation
- Concussion assessment using SCAT3, SAC or other assessment tool
- Serial monitoring and NO Return To Play (RTP) on same day
Treatment
- Physical and cognitive rest until the acute symptoms resolve and then a graded program of exertion prior to medical clearance and RTP
- Graduated RTP (Return To Play) protocol
- 6 step program, each step lasting 24h → RTP in 7 days
- Must be symptoms free 24h to go to next step
- Second impact syndrome.
- Diffuse cerebral edema if the patient experiences a second concussion while still symptomatic from the first concussion → increased ICP → coma/death.
- Rare: 1.5 deaths/yr
- Post-concussion syndrome: persistence of symptoms > 3 months
Gradual RTP (Return To Play) Steps
No activity
Light aerobic exercise
Sport-specific exercise
Non-contact training drills
Full-contact practice
Return to play
Read More
- Developing a decision instrument to guide computed tomographic imaging of blunt head injury patients. https://pubmed.ncbi.nlm.nih.gov/16374287/
- Clinical policy: neuroimaging and decisionmaking in adult mild traumatic brain injury in the acute setting. https://pubmed.ncbi.nlm.nih.gov/19027497/
- The Canadian CT Head Rule for patients with minor head injury. https://pubmed.ncbi.nlm.nih.gov/11356436/
- Indications for Computed Tomography in Patients with Minor Head Injury. https://www.nejm.org/doi/full/10.1056/nejm200007133430204
- Outcomes of urgent warfarin reversal with frozen plasma versus prothrombin complex concentrate in the emergency department. https://pubmed.ncbi.nlm.nih.gov/23770745/
- Immediate and delayed traumatic intracranial hemorrhage in patients with head trauma and preinjury warfarin or clopidogrel use. https://pubmed.ncbi.nlm.nih.gov/22626015/
- Management of minor head injury in patients receiving oral anticoagulant therapy: a prospective study of a 24-hour observation protocol. https://pubmed.ncbi.nlm.nih.gov/22244878/
- Consensus statement on concussion in sport: the 4th International Conference on Concussion in Sport held in Zurich, November 2012. https://bjsm.bmj.com/content/47/5/250