Table of Contents
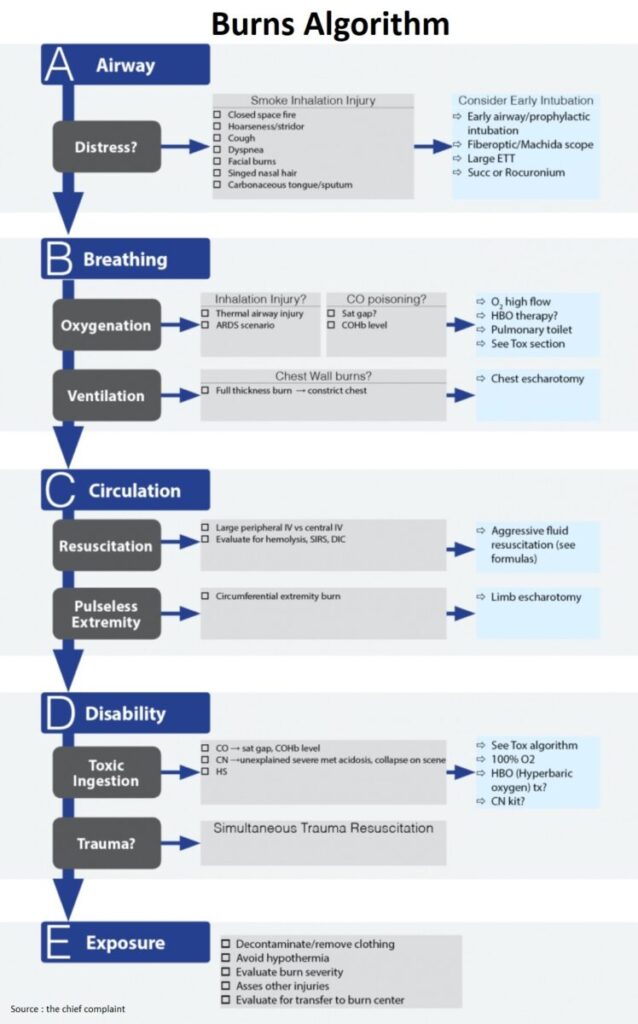
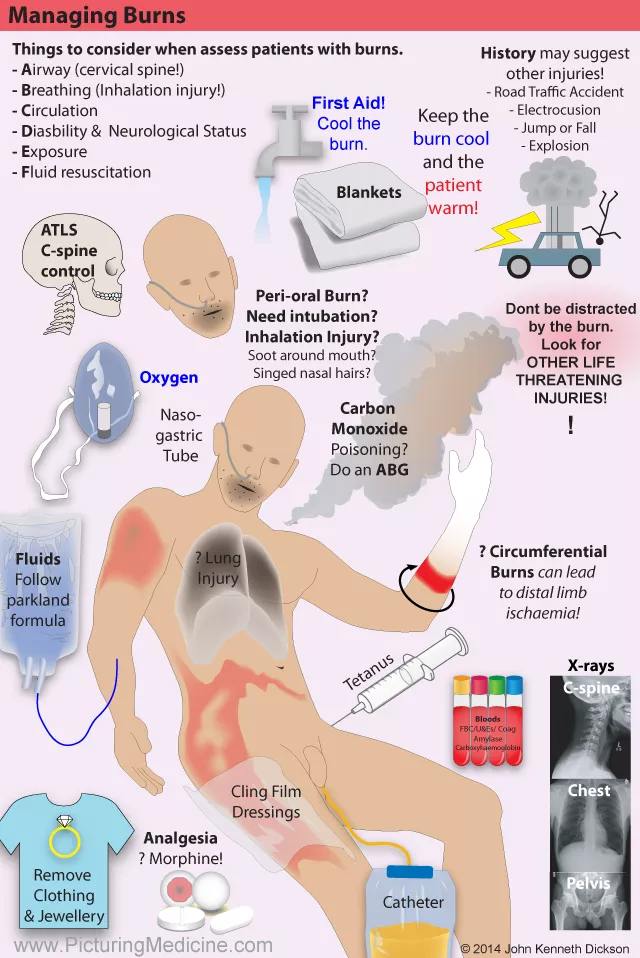
Airway
Respiratory distress
- Consider immediate intubation/airway control
Smoke inhalation injury
- Closed space fire
- Hoarseness/stridor
- Cough, dyspnea
- Facial burns, singed nasal hair/eyebrows
- Carbonaceous tongue/sputum
Major Burn
– Partial thickness: >25% TBSA (adults); >20% TBSA (<10 or >50yo)
– Full thickness > 10 %
– Burns to face, eyes, ears, hands, genitals
– Inhalation injury, major trauma
– Chemical burn, electrical injury
– High risk patients
Treatment
- Timing
- Early airway management is key !
- When in doubt → intubate
- Patient may present well appearing, in no distress → then develop massive facial tongue
- edema minutes to hours → airway nightmare
- RSI Medication
- Ketamine
- Succinylcholine (2mg/kg) permissible
Breathing
Oxygenation
- Inhalation Injury
- Thermal airway injury
- ARDS ?
- CO Poisoning (See Tox section)
- Check for saturation gap (SaO2 significantly less on pulse oximetry than that calculated from the PaO2 on the arterial blood gas), COHb level
Ventilation
- Chest wall burn
- Pathophysiology
- Chest wall constriction → ↓ Low Compliance → ↑ Increase PIP → Unable to ventilate
- Treatment
- Immediate problem: Must treat within a few minutes!
- Chest wall escharotomy
Circulation
Resuscitation
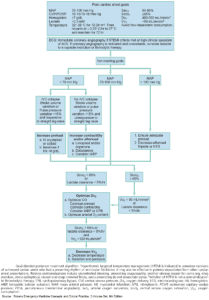
- Fluid resuscitation (Lactated Ringer’s)
- Estimate burn surface area (rule of 9s, palms)
- Increase fluid requirements when inhalation or electrical injury present
- Place foley – should achieve a normal Urinary Output (30-50ml/h in adults)
24h Fluid requirements – Lactated Ringer’s (LR)
– Parkland: 4cc/kg x %TBSA (Total body surface area)
– Consensus: 3cc/kg x %TBSA
– Modified Brooke: 2cc/kg x %TBSA
– Galveston (Peds): 5000ml/m2 x %TBSA + 2000ml
– ALL formulas: ½ fluids in first 8 hours
Pulseless extremity ?
- Circumferential extremity burn
- Pathophysiology
- Burned skin contracts + Subcutaneous swelling → venous occlusion → arterial occlusion → Ischemia
- Treatment
- Limb escharotomy within a few hours
Disability
Trauma
- Trauma present ?
- Assess patient simultaneously for trauma (fall, blast Injury, MVA) and treat (Cervical spine, pneumothorax, internal bleeding !)
- Always attempt to obtain neurologic exam (including rectal/pupil exam) before RSI (rapid sequence intubation)
Toxic inhalation
- CO: saturation gap, COHb level
- CN: unexplained severe metabolic acidosis, collapse on scene
- HS
Exposure
Secondary survey:
- Remove clothing (operative for adherent clothing)
- Stop burning
- Provide first aid (avoid hypothermia with overuse of water to decontaminate wounds)
- Asses for other injuries, asses burn severity (below), consider transfer
Burn Center Transfer (ABA criteria)
– Partial thickness >10% TBSA
– Third degree burns any age group
– Burns to face, hands, feet, genitalia, perineum, major joints
– Electrical burns (including lightning)
– Chemical burns
– Inhalation injury
– Pre-existing medical condition that could complicate management
– Traumatic injury where burn poses greatest risk
General Assessment of Burn Severity (Emerg Med Clin N Am 2007;25:13-146)
- Severity of burn is multifactorial and depends on:
- Depth (use partial and full thickness to describe)
- 1° First degree – epidermal injury, no blister, red, tender, painful (sunburn)
- 2° Second degree – Partial thickness
- i. Superficial (no scar): involves superficial dermis→thin walled fluid blisters
- ii. Deep (+scar): involves reticular dermis →red, blanched white, thick walled blisters
- 3° Third degree – Full thickness: epidermis, dermis → white, leathery, numb
- 4° Fourth degree – Skin, Subcutis, may involve fascia, muscle, bone
- Extent (only 2nd-4th degree)
- Rule of 9s, palms for adults, palms + fingers for children (1%)
- Location: face, eyes, ears, hands, perineum
- Age: mortality = age + TBSA (Total body surface area) (if over 50 yo)
- Etiologic agent (flame, contact, scald, flash, electrical, radiation, chemical)
- Presence of inhalation injury
- Coexisting injury or preexisting illness
- Depth (use partial and full thickness to describe)
- Classify burn according to severity (Major, Moderate, Minor) (AM Coll Surg Bull 1984;69:24)
- Major → need burn center
- Moderate → hospitalize for initial care, not necessarily burn center
- Minor → Outpatient management
Minor Burns
Treatment
- Stop the burning process → Remove clothing (operative for adherent clothing)
- Cool the burn
- Effective within 20 minutes of burn
- Irrigate/immerse in tepid water (15oC) for up to 20 minutes (or soaked gauze)
- Do not use ice
- Analgesia: if severe, may require opioids, then NSAIDs; cover burn
- Cleansing/debridement (Br Med J 1987;295(6591):181)
- New burn is sterile
- Can clean with soap/water or mild antibacterial (chlorhexidine)
- Blisters
- Controversial: can aspirate or de-roof large blisters and remove dead skin or leave alone
- Small blisters should be left alone
- Topical antibiotics
- e.g. Silver sulfadiazene
- Cochrane review: (Cochrane Review 2010)
- No effect on infection
- Slows down healing in patients with partial-thickness burns
- Dressing Layers:
- Layer 1: Non-adherent dressing (xeroform, vaseline gauze, Adaptec)
- Layer 2: Consider antimicrobial layer (Silver sulfadiazene)
- Layer 3: Antishear layer (Kerlix and Ace wrap)
- Tetanus update; No empiric antibiotics
- Follow up: Recheck in 24h and dressing change
Minor Burn
– Partial thickness <15% TBSA adults; <10% (elderly, children)
– Full thickness: <2% TBSA
– No cosmetic/functional risk to eyes, ears, face, hands, perineum
Special types of burns
- Sunburns → if bad, may need IVF, H1/H2 blocker IV, NSAIDs, opiates
- Oral commissure burns (child bites electrical cord) → delayed facial artery bleed
- HF (Hydrofluoric) acid → need aggressive treatment with Ca (topical, IV, intra-arterial)
- Flash burns → may look bad but usually are not (rarely have inhalation injury)
- Electrical burns → may not look bad, but usually are (consider arrhythmias and rhabdomyolysis)
- Usually do not have delayed presentation of Vfib/arrhythmias
- Consider burn center transfer for electrical burns > 1000V
- Tar burns → like dissolves like (use butter, mayo, Bacitracin to remove after cooling)