Table of Contents
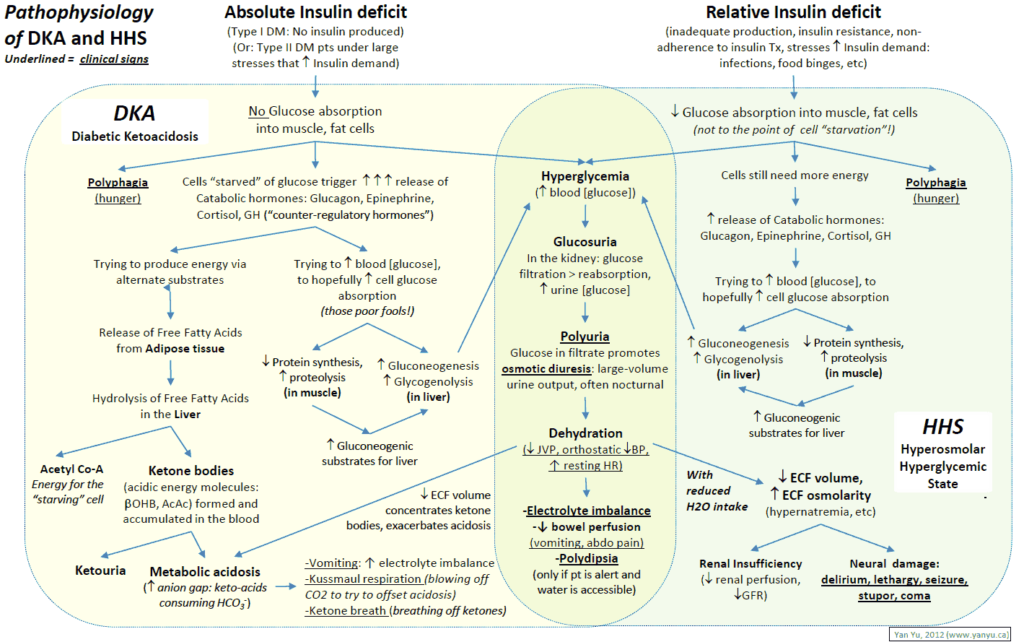
Presentation
- 3Ps – Polyuria, Polydipsia, Polyphagia
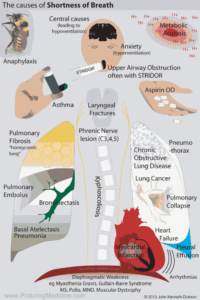
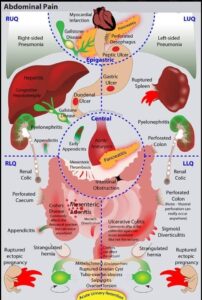
- Non-specific symptoms:
- Weakness, vomiting, abdominal pain, blurry vision
- Physical Exam:
- Acetone smell
- Dehydration / tachycardia / hypotension / shock
- Kussmaul’s respiration (deep/labored breathing secondary to acidosis)
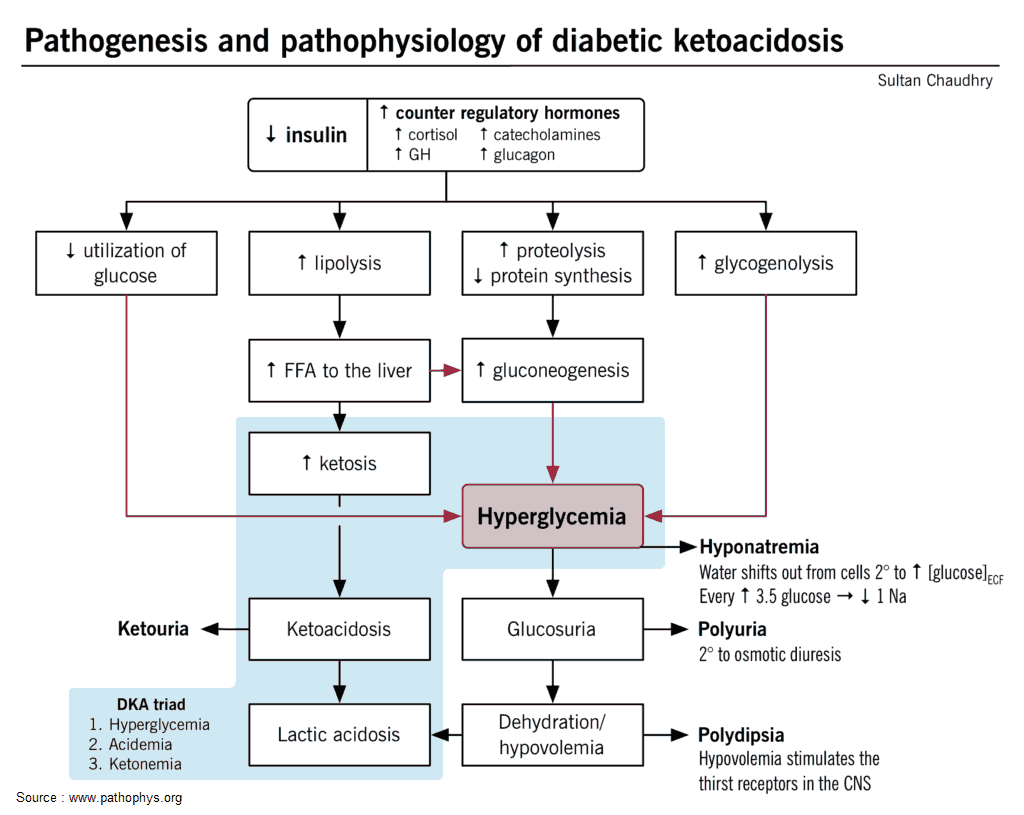
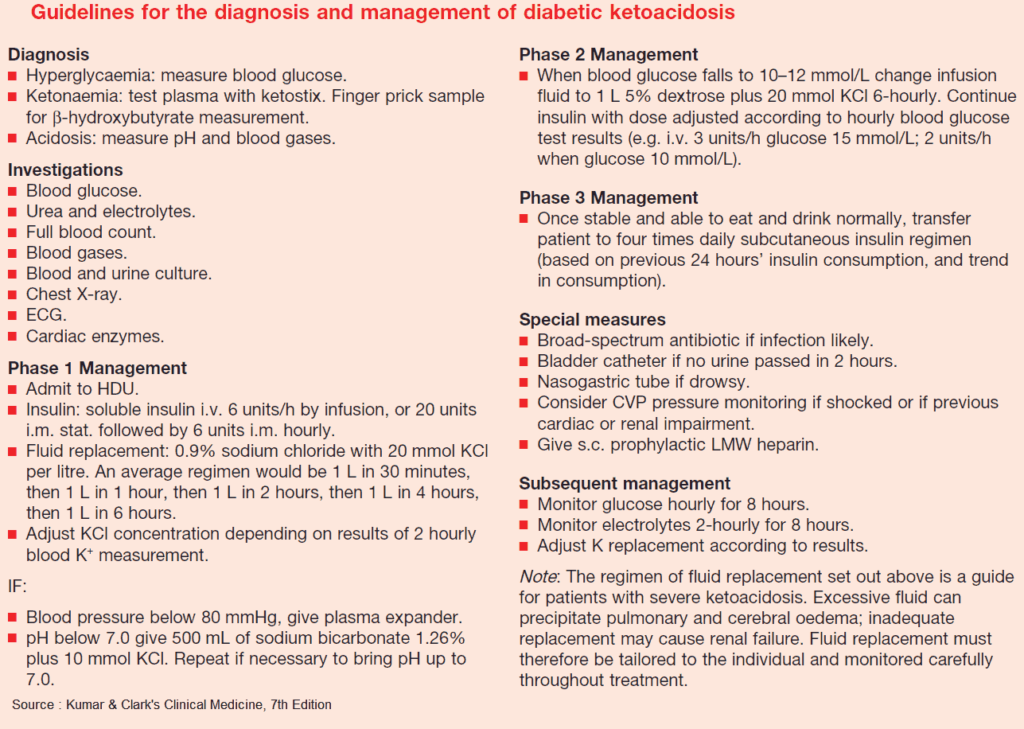
Diagnosis
- DKA diagnostic criteria:
- Hyperglycemia: serum glucose > 250 mg/d
- Acidosis: arterial pH < 7.3, anion gap > 10, serum bicarbonate <18 mEq/l
- Ketosis: ketonuria or ketonemia
- Serum beta-OH-butyrate is the preferred method for measuring ketonemia
DKA Diagnosis
□ D-Diabetes, Blood Sugar > 250
□ K-Ketones in urine/serum
□ A-Acidosis-pH<7.3, HCO3<18
Causes
- Infection (UTI, pneumonia, gastroenteritis, pancreatitis) in 40-50%
- Infarction (ACS, MI)
- Infraction (patient noncompliance with therapy)
- Infant (pregnancy)
- Ischemic (CVA)
- Illegal (alcohol, drug abuse/cocaine abuse)
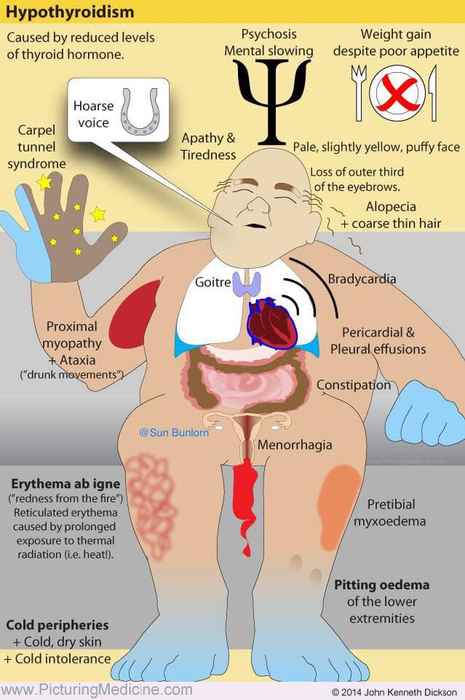
- Iatrogenic (prescription drug interactions, e.g. steroids)
- Idiopathic (new onset type 1 diabetes or other cause)
Treatment
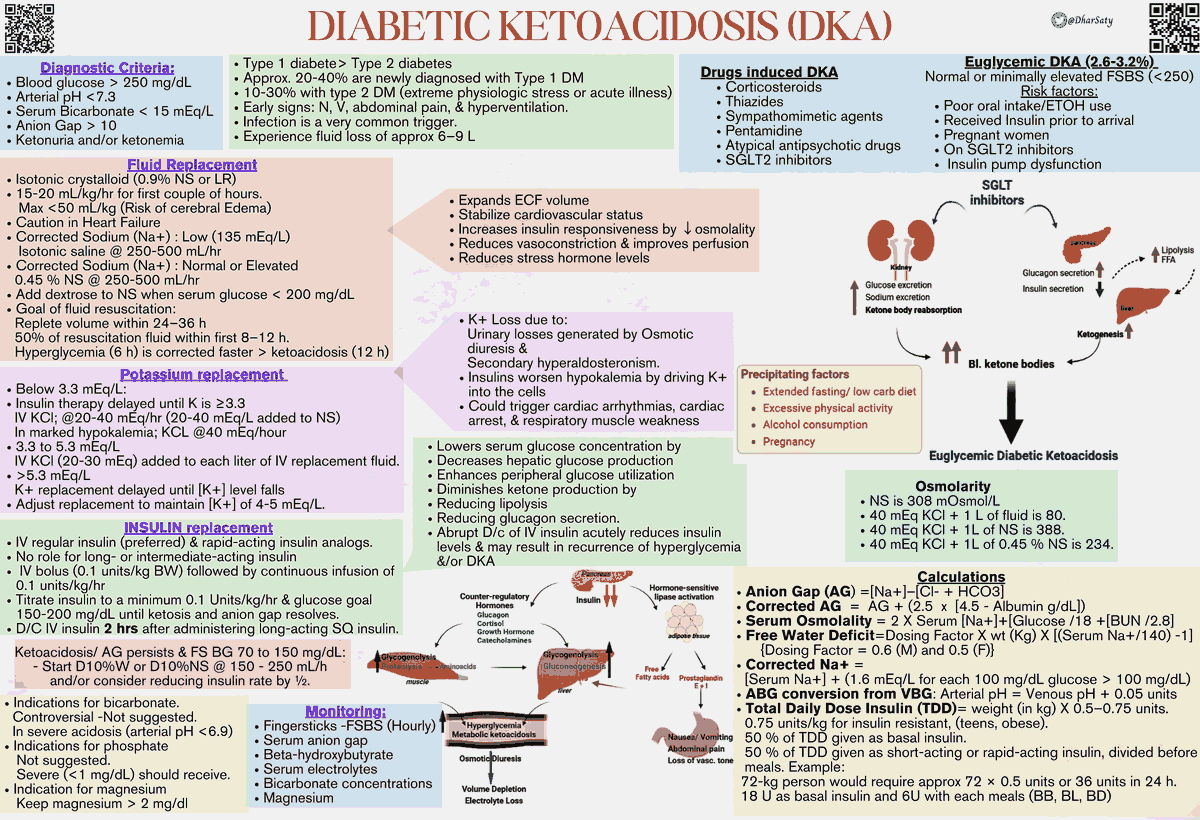
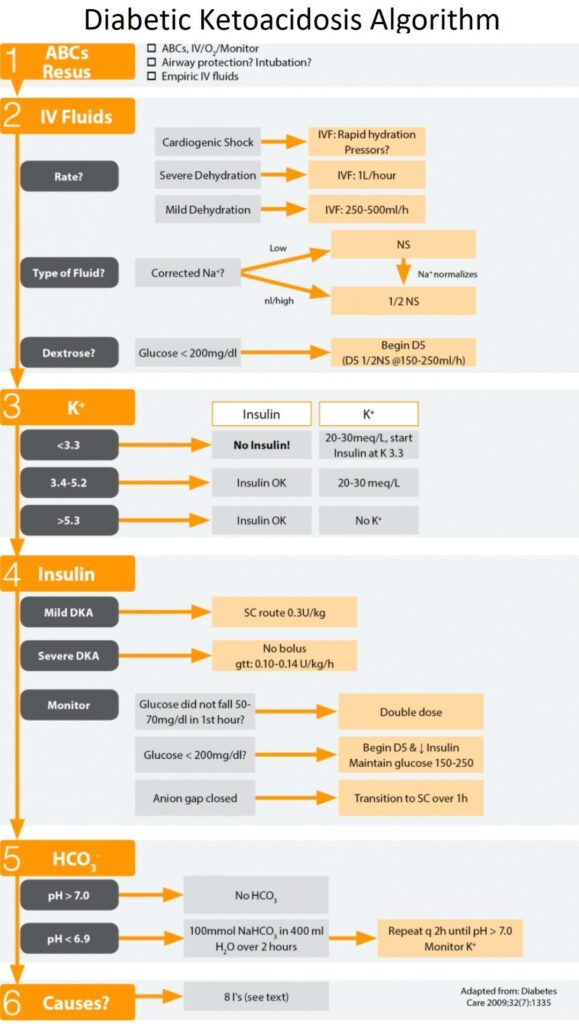
Initial Resuscitation
- Altered sensorium based on level of combination of hyperosmolarity and acidosis (Diabetes Care 2010;33:1837–1839)
- Start with 2L IV Normal Saline empiric before labs
- Start with 2L IV Normal Saline bolus
- Fluid deficit about 100ml/kg (7-8L deficit) secondary to glucose osmotic diuresis
- Can decrease glucose to 300 with IV fluids
Sodium
- Falsely lowered level (hyponatremia) secondary to hyperglycemia
- Correction: Add 1.6 to Na for every 100 over 100 in glucose level
- Corrects with IV Fluids
- 1/2 Normal Saline: Switch to 1/2 NS when Na normalizes
Insulin
- Mechanism of Action: Stops ketogenesis and breakdown of fatty acids
- Caution: Hypokalemia
- Prevalence 5.6% (3 out of 54 patients with hypokalemia) (Am J Emerg Med. 2012;30(3): 481)
- Do not start insulin until you check potassium → if patient hypokalemic, can drop K even more → arrhythmia
- Hold insulin until K>3.3
- Dose: Start 0.1 U/kg/h gtt
- Do not need bolus → insulin bolus not associated with any benefit to patients (J Emerg Med 2010;38(4):422)
- Priming dose of insulin unnecessary if dosing adequately (Diabetes Care 2008;31(11):2081)
- Bolus option dosing: bolus 0.1 U/kg; gtt: 0.1 U/kg/h
- Monitor
- If glucose not decrease by 50mg/dl in first hour → double rate or SQ insulin bolus
- If Glucose >1000 mg/dl, rapid correction puts patient at risk for cerebral edema
- Glucose reaches 200mg/dl:
- i. Reduce Insulin gtt to 0.02-0.05 U/kg/hr or
- ii. Rapid acting insulin 0.1 U/kg SC every 2 hours
- Anion gap closed
- i. Goal: Resolution of acidosis/ketosis (not euglycemia) → do not stop insulin until anion gap closed
- ii. Transition dose SQ insulin (5 Units per 50 over 150-max 20)
- iii. D/C insulin gtt one hour after SQ dose
- Dextrose: When glucose is < 200 mg/dl, add D5 to replacement fluids
- Allows continued insulin administration until ketonemia is controlled while at the same time avoiding hypoglycemia
Potassium
- Total body potassium deficit (average deficit 3-5 meq/kg)
- May see relative hyperkalemia because of acidosis
- Repletion: PO (if able to tolerate) and IV
- Do not start insulin until potassium is > 3.3
HCO3 (Bicarbonate)
- Controversial, recommended by ADA for pH<7.0
- Retrospective studies show no improvement in outcome (Crit Care Med 1999;27:2690)
- No prospective randomized studies concerning the use of bicarbonate in DKA with pH values <6.9 have been reported (Diabetes Care 2002;25:2113–2114)
Other Electrolytes
- Magnesium → depleted secondary to osmotic diuresis, ok to replete
- Phosphorus → may precipitously drop with treatment of DKA, must replete
Monitoring
- Glucose q 1 hour
- pH and electrolytes q 2-4h
- ABG not needed, VBG is adequate for monitoring (Emerg Med J 2006;23(8):622)
Complications
- Hypoglycemia – overzealous DKA treatment
- Hyperglycemia – undertreatment
- Hypokalemia
- Caused by insulin tx, correction of acidosis and volume expansion
- Return of DKA (Must bridge with SQ insulin dose)
- Hyperchloremia
- Cerebral Edema
- Prognosis: mortality (20-50%), 1/3 survivors in vegetative state
- Risk factors: age < 5, new onset DM
- Symptoms: Depressed LOC/AMS (Altered Mental Status), pupillary changes, seizures
- Treatment
- Mannitol 1-2 gm/kg
- Consider: Intubation, Dexamethasone, hypertonic saline (5-10ml/kg)
Read Also : Pitfalls in the Management of Diabetic Ketoacidosis (DKA)
References
- Kitabchi AE, Umpierrez GE, Miles JM, Fisher JN. Hyperglycemic crises in adult patients with diabetes. Diabetes Care. 2009 Jul;32(7):1335-43. doi: 10.2337/dc09-9032. PMID: 19564476; PMCID: PMC2699725. (https://pubmed.ncbi.nlm.nih.gov/19564476/)
- Nyenwe EA, Razavi LN, Kitabchi AE, Khan AN, Wan JY. Acidosis: the prime determinant of depressed sensorium in diabetic ketoacidosis. Diabetes Care. 2010 Aug;33(8):1837-9. doi: 10.2337/dc10-0102. Epub 2010 May 18. PMID: 20484127; PMCID: PMC2909073. https://pubmed.ncbi.nlm.nih.gov/20484127/
- Arora S, Cheng D, Wyler B, Menchine M. Prevalence of hypokalemia in ED patients with diabetic ketoacidosis. Am J Emerg Med. 2012 Mar;30(3):481-4. doi: 10.1016/j.ajem.2011.01.002. Epub 2011 Feb 11. PMID: 21316179. https://pubmed.ncbi.nlm.nih.gov/21316179/
- Goyal N, Miller JB, Sankey SS, Mossallam U. Utility of initial bolus insulin in the treatment of diabetic ketoacidosis. J Emerg Med. 2010 May;38(4):422-7. doi: 10.1016/j.jemermed.2007.11.033. Epub 2008 Jun 2. PMID: 18514472. https://pubmed.ncbi.nlm.nih.gov/18514472/
- Kitabchi AE, Murphy MB, Spencer J, Matteri R, Karas J. Is a priming dose of insulin necessary in a low-dose insulin protocol for the treatment of diabetic ketoacidosis? Diabetes Care. 2008 Nov;31(11):2081-5. doi: 10.2337/dc08-0509. Epub 2008 Aug 11. PMID: 18694978; PMCID: PMC2571050. https://pubmed.ncbi.nlm.nih.gov/18694978/
- Viallon A, Zeni F, Lafond P, Venet C, Tardy B, Page Y, Bertrand JC. Does bicarbonate therapy improve the management of severe diabetic ketoacidosis? Crit Care Med. 1999 Dec;27(12):2690-3. doi: 10.1097/00003246-199912000-00014. PMID: 10628611. https://pubmed.ncbi.nlm.nih.gov/10628611/
- Latif KA, Freire AX, Kitabchi AE, Umpierrez GE, Qureshi N. The use of alkali therapy in severe diabetic ketoacidosis. Diabetes Care. 2002 Nov;25(11):2113-4. doi: 10.2337/diacare.25.11.2113. PMID: 12401775. https://pubmed.ncbi.nlm.nih.gov/12401775/
- Middleton P, Kelly AM, Brown J, Robertson M. Agreement between arterial and central venous values for pH, bicarbonate, base excess, and lactate. Emerg Med J. 2006 Aug;23(8):622-4. doi: 10.1136/emj.2006.035915. PMID: 16858095; PMCID: PMC2564165. https://pubmed.ncbi.nlm.nih.gov/16858095/