Table of Contents
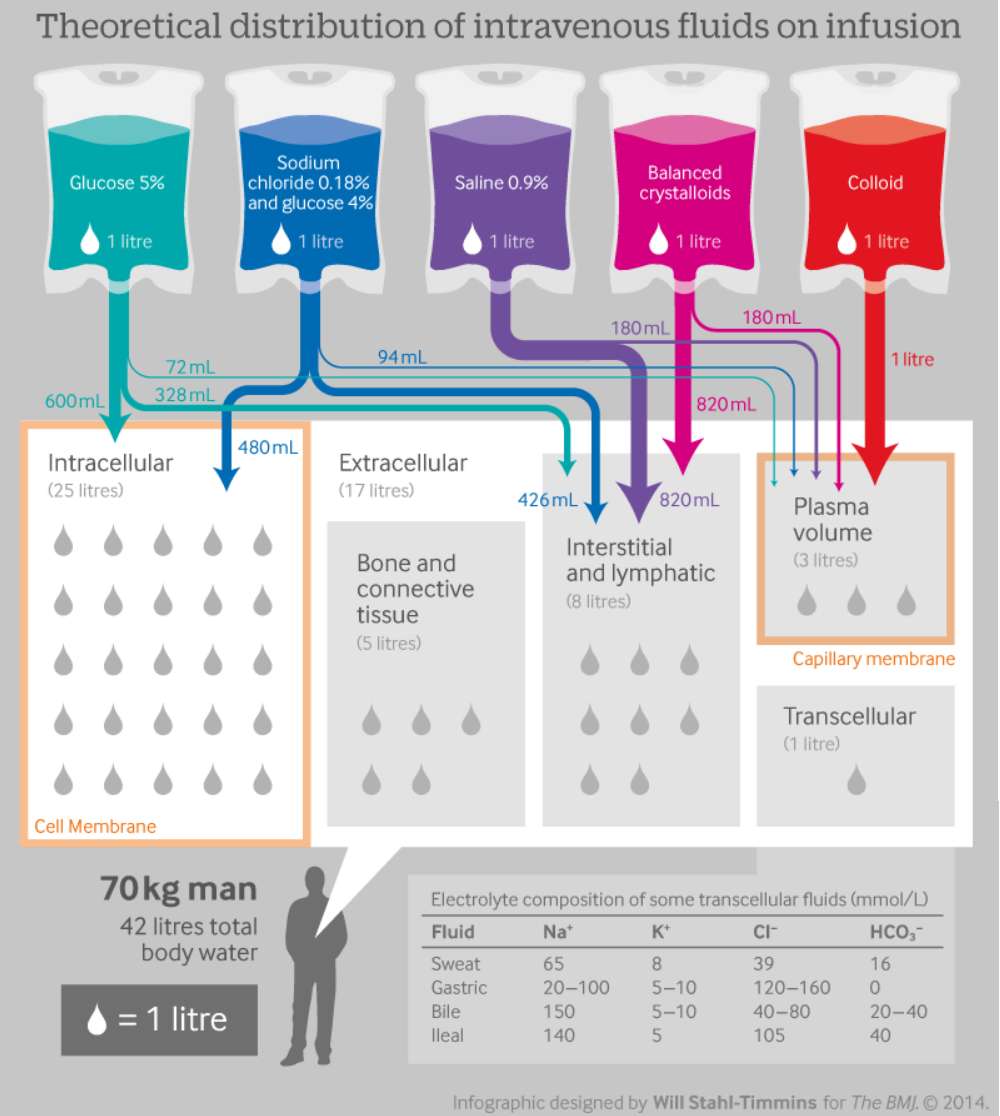
For an average adult, water accounts for 60% of total body mass. However, this percentage decreases as the percentage of fat increases since fat has a lower water content than lean tissue. For a normal, healthy 70-kg adult, daily water intake should be between 2,000 and 3,000 mL to make up for urinary and insensible losses.
Total body water is partitioned between intracellular and extracellular fluid compartments. Water moves from the compartment of low osmolality to that of higher osmolality until the fluids on either side of the barrier share the same osmolality. If this redistribution of water is too excessive or rapid, then the corresponding changes in cell volume can lead to cellular dysfunction or injury. This disruption in fluid balance can be from hemorrhagic or nonhemorrhagic volume losses.
Some of the most commonly treated conditions in the emergency department (ED) requiring intravenous (IV) fluid resuscitation include :
- trauma,
- gastrointestinal (GI) losses,
- sepsis,
- diabetic ketoacidosis (DKA)
- hyperosmolar hyperglycemic state (HHS),
- hyponatremia,
- rhabdomyolysis,
- burns.
Types of Fluid
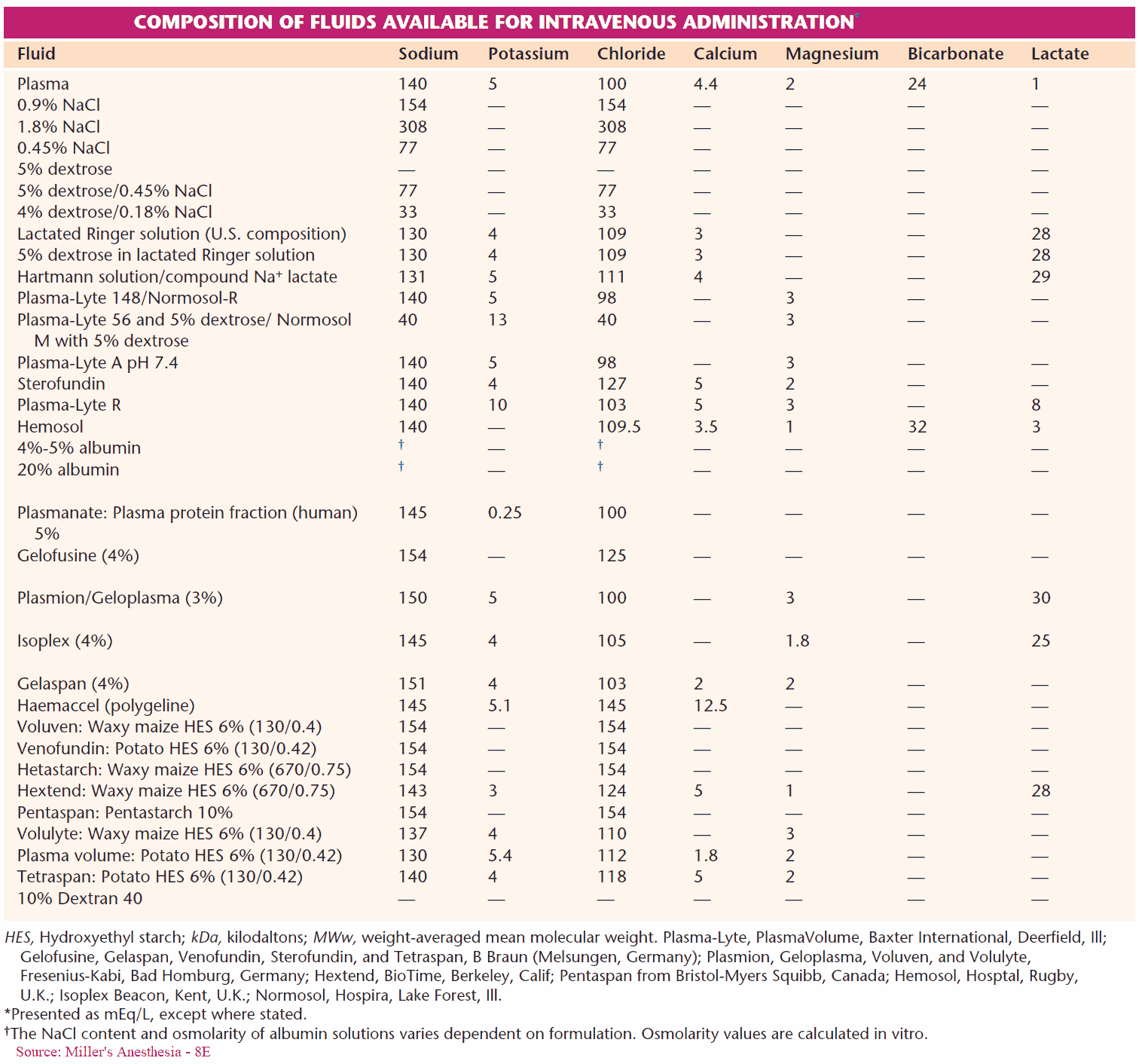
Fluids are classified according to molecular weight and oncotic pressure. Crystalloids have a lower molecular weight and lower oncotic pressure compared to colloids.
Colloids preserve oncotic pressure and their vascular retention makes them more efficient volume expanders with a longer duration of action than crystalloids. However, when dosed appropriately, isotonic crystalloid solutions like lactated Ringer’s (LR) or normal saline (NS) are equally effective volume expanders. Therefore, with few exceptions, there appears to be no proven clinical superiority to using colloids over crystalloids.
Considering the significant cost advantage and availability, crystalloid solutions are the most commonly used resuscitation fluid in the ED.
Fluids in Hemorrhage
Total body fluid loss due to hypovolemia can be from trauma, hemorrhage, or GI losses. Patients experiencing uncontrolled hemorrhagic shock should be treated with deliberate hypotensive fluid resuscitation, as overaggressive resuscitation can exacerbate their ongoing bleeding by interrupting formed thrombus.
Efforts should be focused on getting the patient to surgery to identify and stop the bleed. For patients in controlled hemorrhagic shock where the bleeding site has been identified and stopped, fluid resuscitation is aimed at normalizing their hemodynamics. In both cases, the choice of fluids is pRBCs, FFP, and platelets given at a ratio of 1:1:1.
Fluids in GI Losses
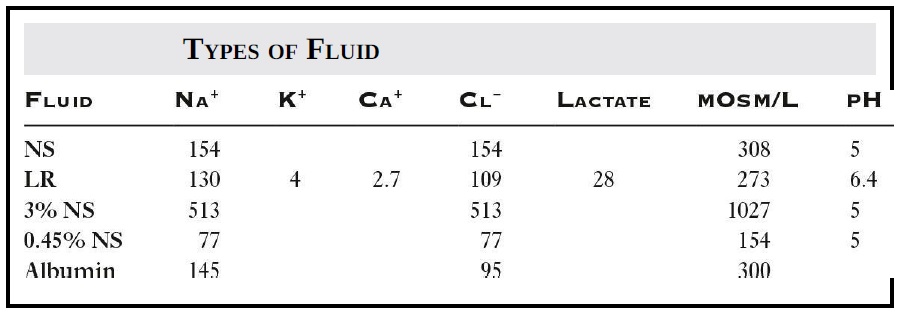
Patients with GI losses from profuse vomiting, gastric outlet obstruction, and nasogastric suctioning develop a hypochloremic metabolic alkalosis. In these patients, the best choice is NS as it contains a higher concentration of chloride. Patients with diarrhea requiring IV fluid resuscitation should receive LR as it better corrects the hyperchloremic metabolic acidosis they can develop.
Fluids in Septic Shock
Patients in septic shock require aggressive IV fluid resuscitation. The preferred fluid is crystalloid as randomized trials and meta-analyses have found increased cost with no clear benefit with the use of colloids.
Fluids in DKA and HHS
Patients in DKA or HHS require careful electrolyte and fluid replacement and the choice of resuscitation fluid depends upon the patient’s initial state of hydration, blood pressure, and sodium, potassium, and glucose concentrations In general, the recommended initial resuscitation fluid is NS. The suggested amount is 1 to 1.5 L given during the first hour, adjusted accordingly depending upon the patient’s clinical state. Subsequent fluids should be either 0.45% NS or LR to prevent hyperchloremic metabolic acidosis.
Dextrose should be added when the serum glucose level reaches 200 mg/dL in DKA or 250 to 300 mg/dL in HHS. Adequate fluid resuscitation will result in an increased response to insulin. Cerebral edema may develop if the osmolality is reduced too rapidly; however, this is more of a concern in the pediatric patient.
Fluids for Hyponatremia
Treatment of hyponatremia varies based on duration, sodium level, volume status, and symptoms. The overall goal is to increase serum sodium by 4 to 6 mEq/L over the first several hours, but not to exceed 8 mEq/L in any 24-hour period to avoid the risk of central pontine myelinolysis.
Acute, severe hyponatremia (sodium < 120 mEq/L) presenting with altered mental status, seizures, or coma should be treated emergently with 3% hypertonic saline with initial 100-mL bolus given over 10 minutes followed by another 100 mL over the next 50 minutes; then reassess. Each 100-mL bolus will raise sodium by 2 to 3 mEq/L.
Asymptomatic patients with acute or hyperacute severe hyponatremia should receive 3% hypertonic saline at a rate of 0.5 to 2 mL/kg/h. For patients with moderate to severe hyponatremia from SIADH or in hypervolemic state, the initial first-line treatment is fluid restriction with a goal of 500 mL/d below the 24-hour urine volume. NS is not the preferred emergent choice as it will raise the serum sodium slower than hypertonic saline and patients with SIADH do not respond well to it.
Fluids for Rhabdomyolysis
Rhabdomyolysis requires early and aggressive fluid resuscitation to prevent acute kidney injury (AKI) and increase urinary potassium excretion. The initial treatment is NS at a rate of 1 to 2 L/h. Patients who have a stable plasma CK (creatine kinase) < 5,000 units/L do not require IV fluid, as studies have shown the risk of AKI is low.
The use of chloride-restrictive fluid (LR) instead of NS has been reported to decrease the incidence of AKI; however, there are no studies that directly compare the efficacy and safety of different types and rates of fluid administration in this setting.
Fluids for Burns
Patients with superficial deep and full-thickness burns >30% of total body surface area should receive fluid resuscitation with LR. The Parkland formula is used to guide acute resuscitation, with continued reassessments using urine output and hemodynamics to make any alterations as needed. After the first 8 hours, if the patient is continuing to require large volumes of fluid, albumin can be substituted for 1/3 of the crystalloid, remembering to adjust the dose of albumin where 1 cc of albumin is equivalent to 3 cc of crystalloid.
Complications
The major complications from improper management of IV fluid resuscitation are inadequate or excessive volume replacement, electrolyte abnormalities, and hematologic complications.
Key Points
- With few exceptions, there appears to be no proven clinical superiority to using colloids over crystalloids.
- Patients with GI losses from profuse vomiting, gastric outlet obstruction, and nasogastric suctioning develop a hypochloremic metabolic alkalosis. In these patients, the best choice is normal saline.
- Patients with diarrhea requiring IV fluid resuscitation should receive LR as it better corrects the hyperchloremic metabolic acidosis they can develop.
- Rhabdomyolysis requires early and aggressive fluid resuscitation to prevent AKI and increase urinary potassium excretion. The initial treatment is NS at a rate of 1 to 2 L/h.
- DKA or HHS requires careful electrolyte and fluid replacement; the recommended initial resuscitation fluid is NS at 1 to 1.5 L given during the first hour, adjusted accordingly depending upon the patient’s clinical state.