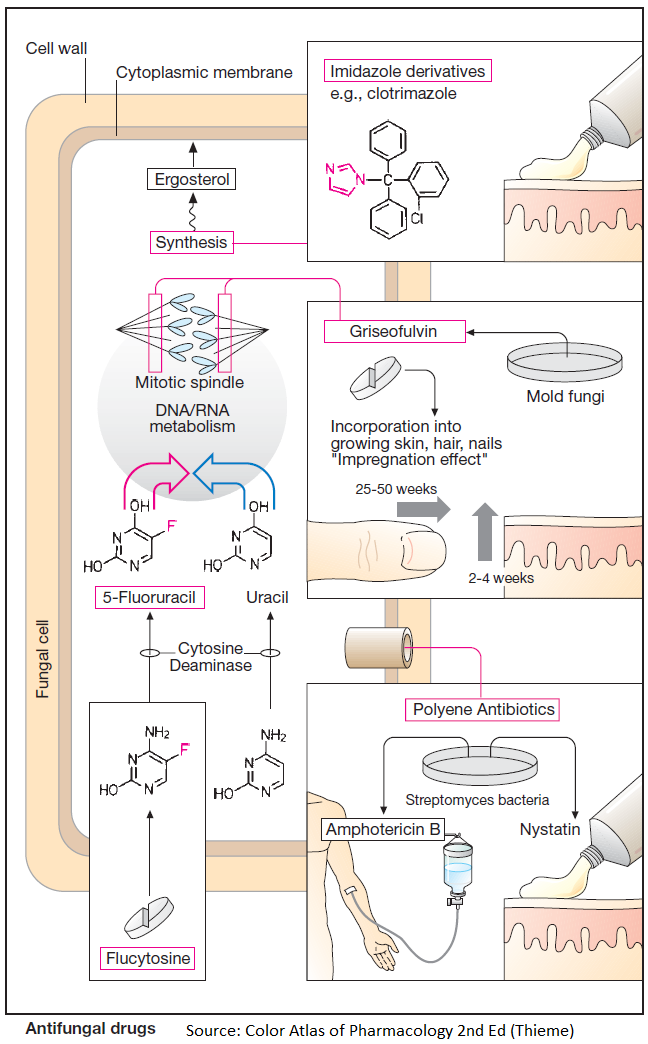
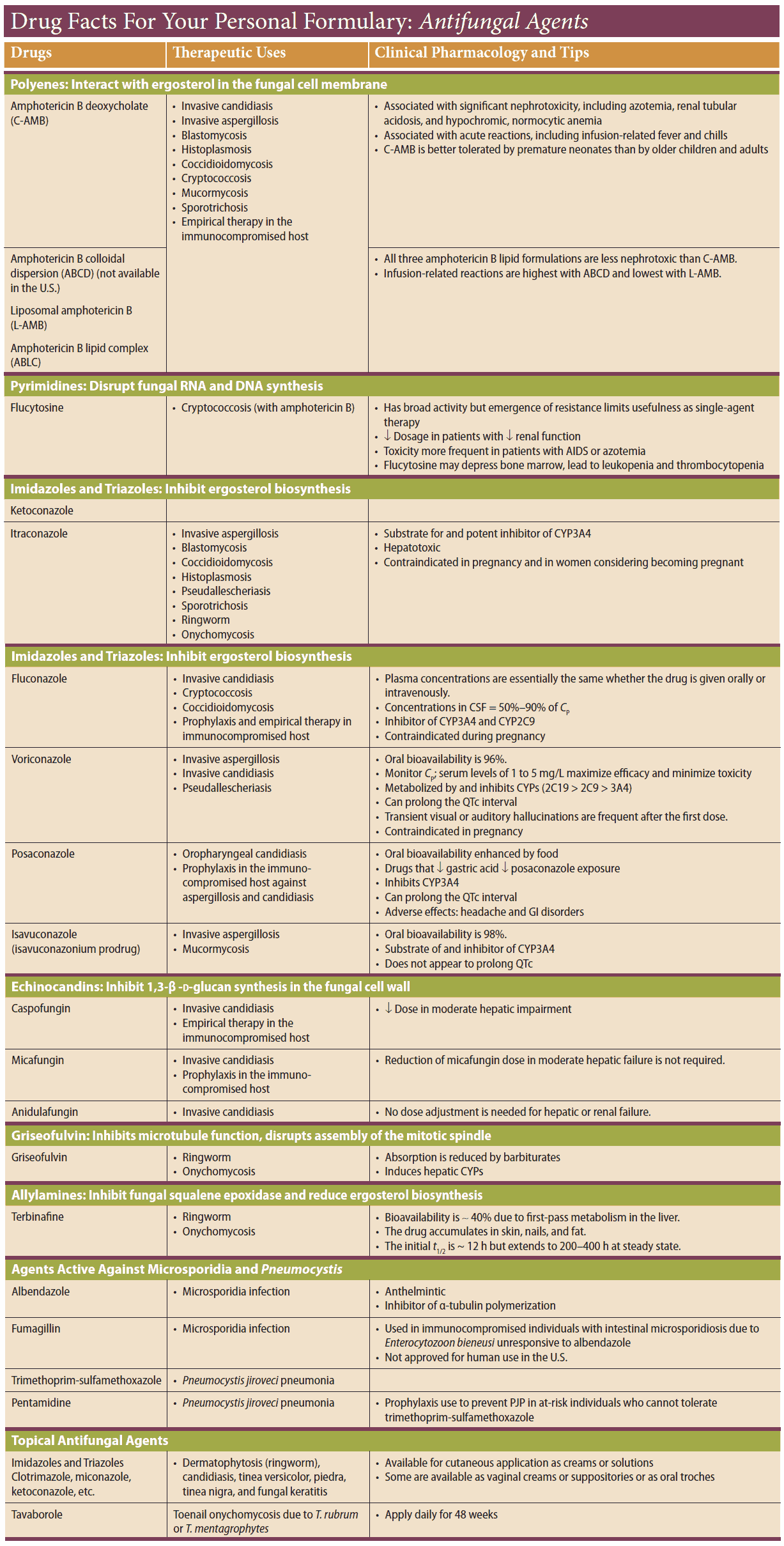
Infections due to fungi are usually confined to the skin or mucous membranes: local or superficial mycosis. However, in immune deficiency states, internal organs may also be affected: systemic or deep mycosis.
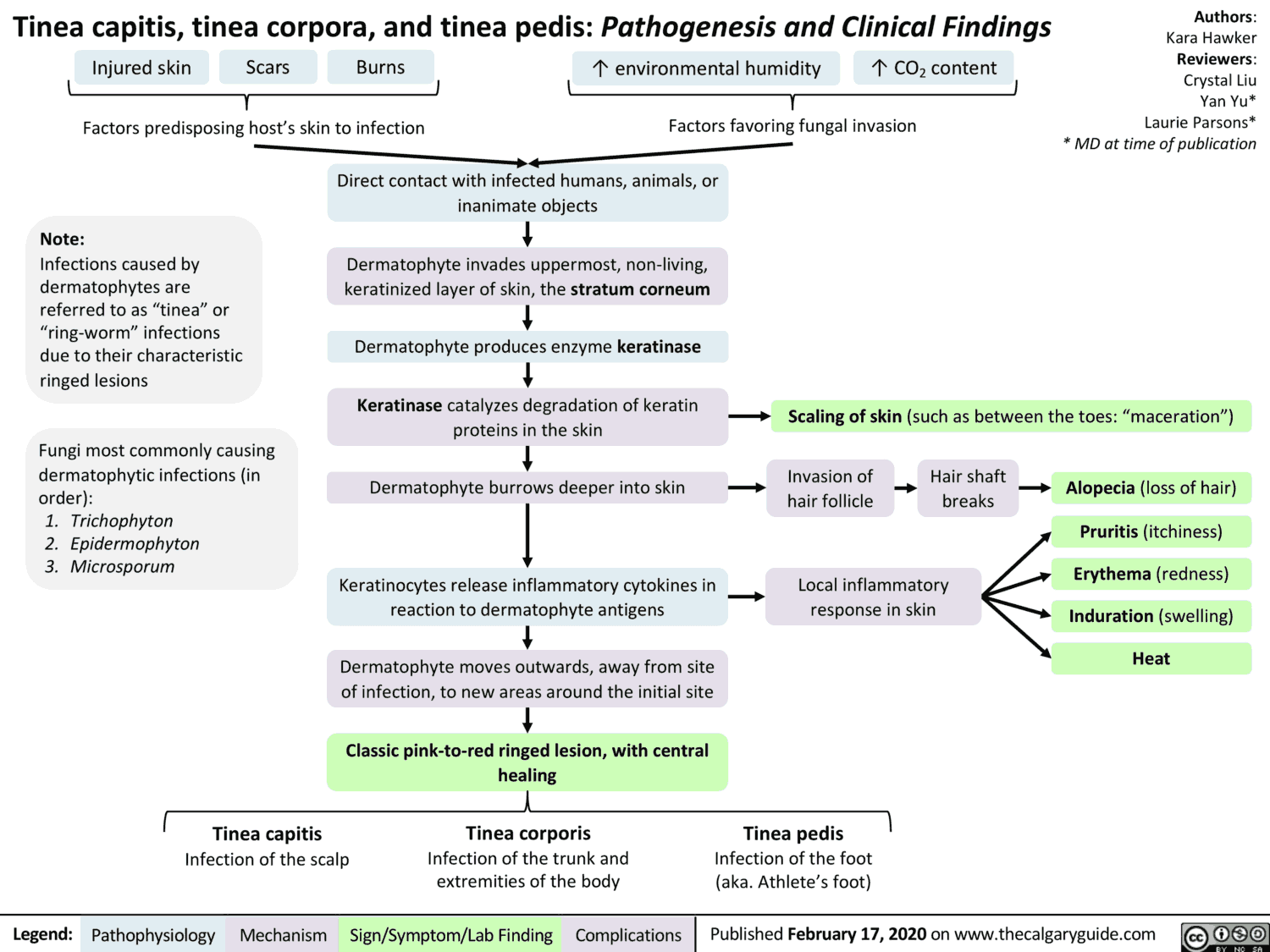
Mycoses are most commonly due to dermatophytes, which affect the skin, hair, and nails following external infection.
Candida albicans, a yeast organism normally found on body surfaces, may cause infections of mucous membranes, less frequently of the skin or internal organs when natural defenses are impaired (immunosuppression, or damage of microflora by broad-spectrum antibiotics).
Imidazole Derivatives
- Clotrimazole
- Miconazole
- Ketoconazole
- Fluconazole
- Itraconazole
- Econazole oxiconazole
- Isoconazole
- Bifonazole
Imidazole derivatives inhibit ergosterol synthesis. This steroid forms an integral constituent of cytoplasmic membranes of fungal cells, analogous to cholesterol in animal plasma membranes.
Fungi exposed to imidazole derivatives stop growing (fungistatic effect) or die (fungicidal effect). The spectrum of affected fungi is very broad. Because they are poorly absorbed and poorly tolerated systemically, most imidazoles are suitable only for topical use (clotrimazole, econazole oxiconazole, isoconazole, bifonazole, etc.). Rarely, this use may result in contact dermatitis.
Miconazole is given locally, or systemically by short-term infusion (despite its poor tolerability). Because it is well absorbed, ketoconazole is available for oral administration.
Fluconazole and itraconazole are newer, orally effective triazole derivatives. The topically active allylamine naftidine and the morpholine amorolfine also inhibit ergosterol synthesis, albeit at another step.
Adverse Effects of Imidazole Derivatives
Adverse effects are rare; however, the possibility of fatal liver damage should be noted. Remarkably, ketoconazole may inhibit steroidogenesis (gonadal and adrenocortical hormones).
Polyene Antibiotics
The polyene antibiotics, amphotericin B and nystatin, are of bacterial origin. They insert themselves into fungal cell membranes (probably next to ergosterol molecules) and cause formation of hydrophilic channels. The resultant increase in membrane permeability, e.g., to K+ ions, accounts for the fungicidal effect.
Amphotericin B
Amphotericin B is active against most organisms responsible for systemic mycoses. Because of its poor absorbability, it must be given by infusion, which is, however, poorly tolerated (chills, fever, CNS disturbances, impaired renal function, phlebitis at the infusion site).
Applied topically to skin or mucous membranes, amphotericin B is useful in the treatment of candidal mycosis. Because of the low rate of enteral absorption, oral administration in intestinal candidiasis can be considered a topical treatment.
Nystatin
Nystatin is used only for topical therapy.
Flucytosine
Flucytosine is converted in candida fungi to 5-fluorouracil by the action of a specific cytosine deaminase. As an antimetabolite, this compound disrupts DNA and RNA synthesis, resulting in a fungicidal effect.
Given orally, flucytosine is rapidly absorbed. It is well tolerated and often combined with amphotericin B to allow dose reduction of the latter.
Griseofulvin
Griseofulvin originates from molds and has activity only against dermatophytes. Presumably, it acts as a spindle poison to inhibit fungal mitosis. Although targeted against local mycoses, griseofulvin must be used systemically.
It is incorporated into newly formed keratin. “Impregnated” in this manner, keratin becomes unsuitable as a fungal nutrient. The time required for the eradication of dermatophytes corresponds to the renewal period of skin, hair, or nails.
Griseofulvin may cause uncharacteristic adverse effects. The need for prolonged administration (several months), the incidence of side effects, and the availability of effective and safe alternatives have rendered griseofulvin therapeutically obsolete.