Table of Contents
- Pulmonary hypertension (PH) can be caused by a myriad of vascular, pulmonary, cardiac, and rheumatologic conditions.
- Pulmonary hypertension is defined as a mean pulmonary artery pressure (PAP) greater than or equal to 25 mm Hg at rest measured by right heart catheterization (RHC).
- Although echocardiography can be helpful for initial evaluation of PH, the gold standard for diagnosis remains right heart catheterization (RHC).
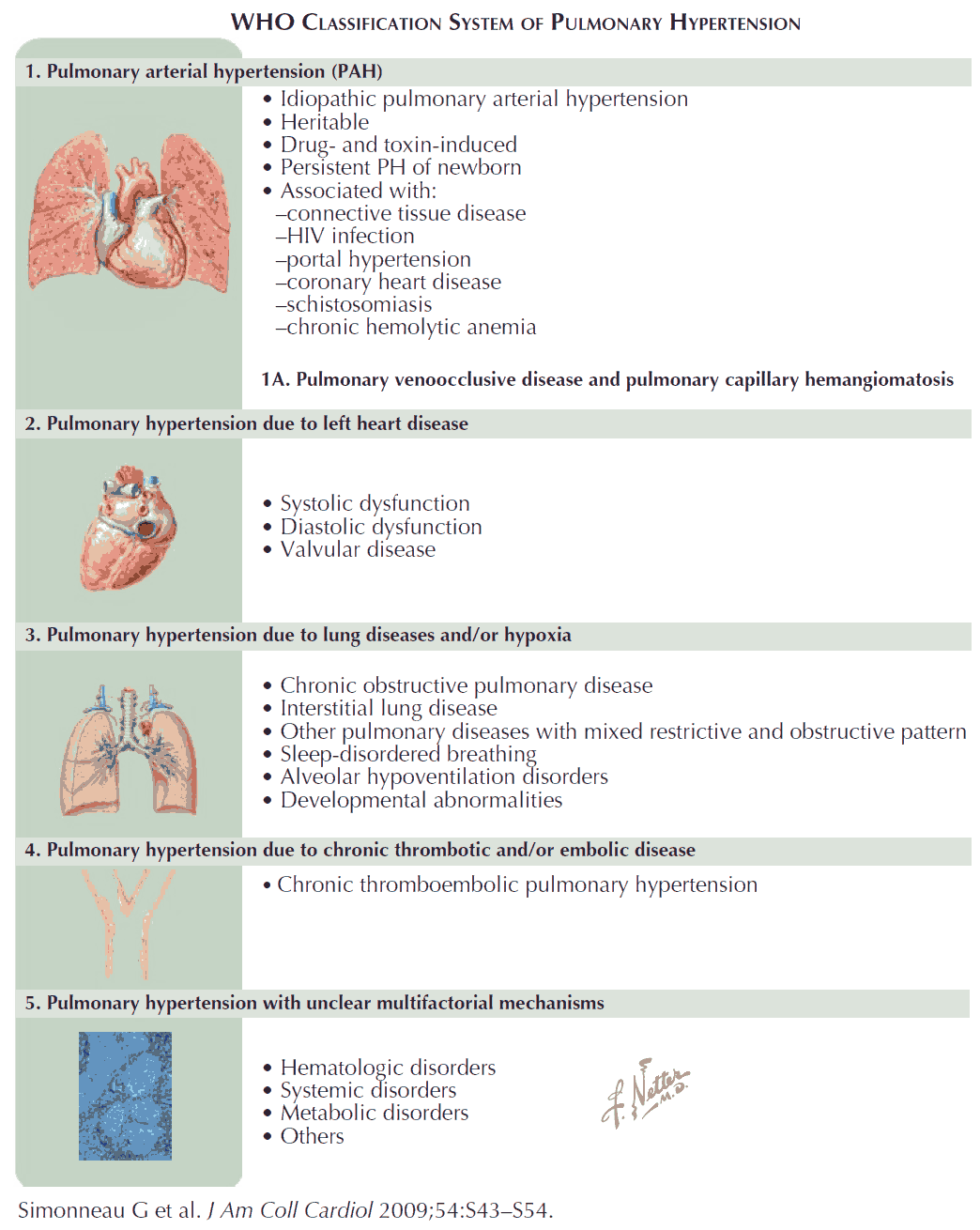
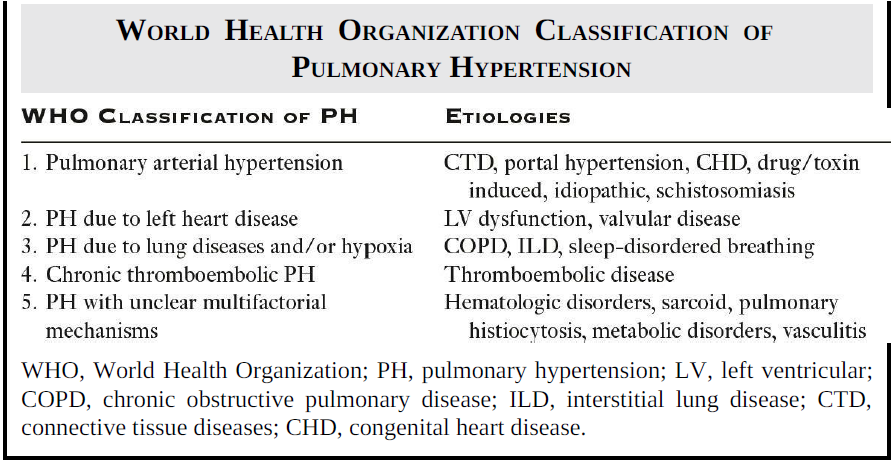
- The World Health Organization (WHO) divides PH into five groups based on the etiology.
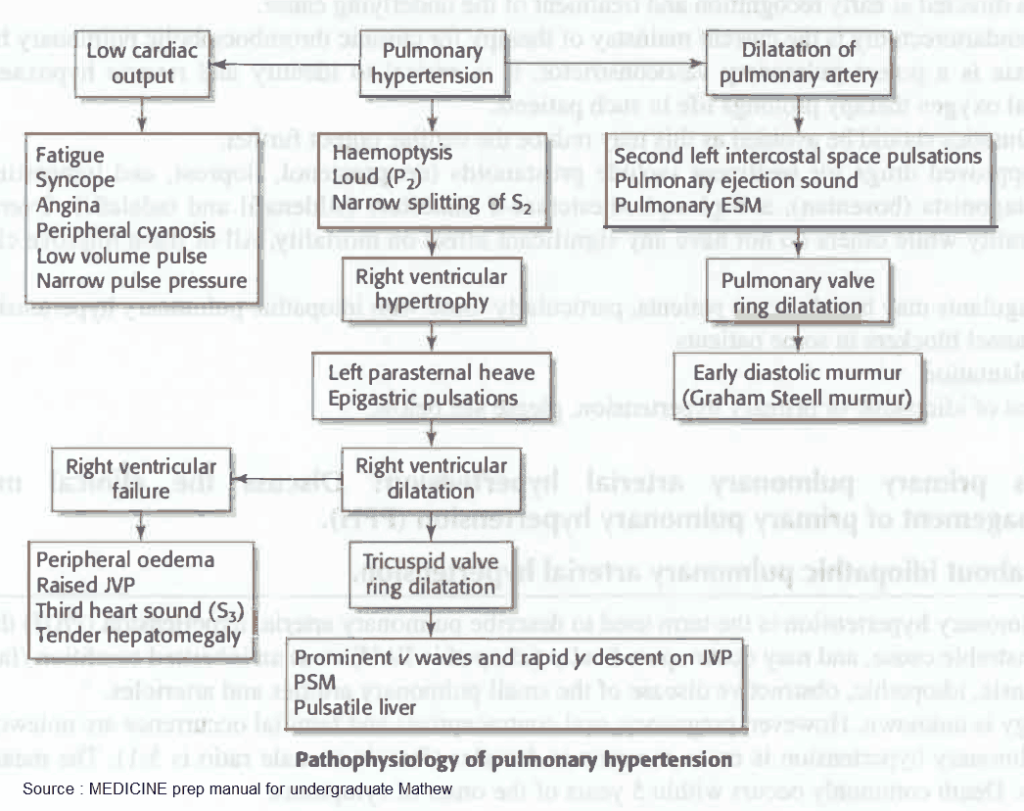
Pathophysiology
The primary pathophysiologic event in PH is pulmonary vascular proliferation that results in a progressive increase in pulmonary vascular resistance (PVR).
The right ventricle (RV) is a thin-walled structure with limited ability to adapt to the increase in PVR. Eventually, the RV becomes dilated with decreased contractility. In addition, RV dilatation displaces the interventricular septum into the left ventricle (LV) and impedes cardiac output. The end result is progressive RV failure.
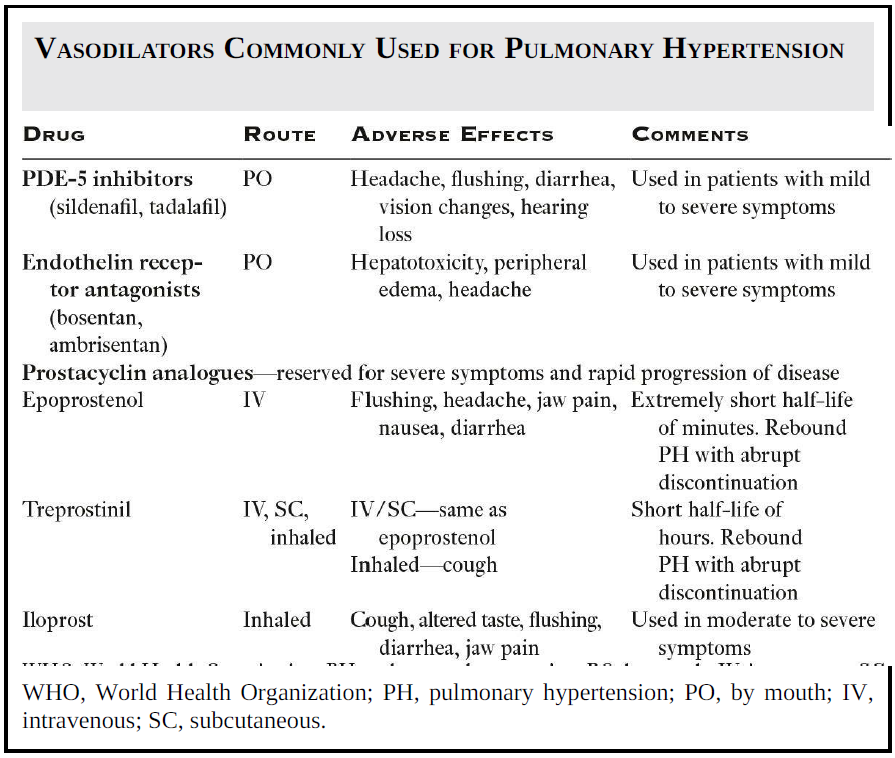
The mainstay of chronic treatment for PH remains supplemental oxygen, diuretic medications, and treatment of the underlying cause. WHO Group 1 PH is a rare disease with a unique pathophysiology and is often treated with pulmonary vasodilators. Vasodilator therapy has not been found to be beneficial in other WHO Groups.
Symptoms and Signs of Pulmonary Hypertension
Patients with PH often present to the emergency department (ED) with acute RV failure. Clinically, decompensated disease manifests with signs and symptoms that include:
- dyspnea
- hypoxia
- syncope
- chest pain
- lower extremity edema.
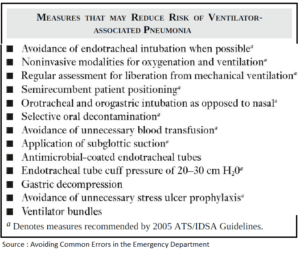
Sudden deterioration in RV function can rapidly lead to shock, cardiovascular collapse, and death. In the ED, it is important to rapidly recognize and treat common precipitants of acute decompensation. These include sepsis, tachyarrhythmias, hypoxia, pulmonary embolism (PE), and the abrupt withdrawal of vasodilator medications.
Common Precipitants of Acute Decompensation
1. Sepsis in Pulmonary Hypertension
Sepsis is a common cause of acute decompensation in PH patients that requires prompt recognition and treatment. It often results from bacterial translocation from the gut due to bowel edema and ischemia from chronic RV dysfunction.
Central venous catheters used to administer intravenous vasodilators are another source of infection. Although systemic vasodilatation occurs in sepsis, the pulmonary circulation tends to have an increase in vascular tone, which can worsen RV function. Sepsis-induced hypovolemia and acidosis can also worsen RV function.
2. Tachyarrhythmias in Pulmonary Hypertension
Supraventricular tachyarrhythmias (i.e., atrial fibrillation, atrial flutter) are commonly seen in patients with PH and are poorly tolerated. Atrial contraction is important to both RV and LV diastolic filling in severe PH. Maintenance of sinus rhythm, rather than simply rate control, is of utmost importance.
Agents used to treat tachyarrhythmias have negative inotropic properties (i.e., calcium channel blockers, beta-blockers) and may worsen RV function. As a result, agents such as amiodarone and digoxin are often used for atrial fibrillation. Electrical cardioversion may be required to restore sinus rhythm in many patients.
3. Pulmonary Embolism in Pulmonary Hypertension
Patients with PH are at high risk of PE. Even a small PE can cause a precipitous increase in the PAP and trigger RV failure in patients with severe PH. Emergency providers should maintain a high suspicion of PE in this population.
Immediate treatment with thrombolytic medications or embolectomy may be required to reverse the sudden increase in PAP and avoid cardiovascular collapse.
4. Hypoxia in Pulmonary Hypertension
Hypoxia is a potent trigger of pulmonary vasoconstriction. In patients with PH, hypoxic vasoconstriction can acutely elevate the PAP and result in RV failure.
Rapid and aggressive correction of hypoxemia with supplemental oxygen is important in patients with severe PH.
5. Abrupt Withdrawal of Vasodilator Medications
The abrupt discontinuation of vasodilator medications can result in a rebound increase in the PAP and precipitate RV failure.
Epoprostenol has a half-life of minutes and is typically administered via a continuous infusion. Central line or pump malfunction can result in abrupt discontinuation of these medications. Such an event should be treated as a medical emergency and the infusion restarted promptly via alternate means if necessary.
Key Points
- Sepsis is a common cause of acute RV deterioration in patients with PH.
- PH patients do not tolerate atrial arrhythmias well. Electrical cardioversion may be needed to restore sinus rhythm.
- Administer supplemental oxygen to hypoxic patients with PH.
- Immediately restart continuous vasodilator infusions, most notably epoprostenol.
- Even small PEs can result in significant deterioration in the patient with severe PH.