The rhythm is irregularly irregular at an average rate of 156 bpm. There are only three rhythms that are irregularly irregular:
- sinus arrhythmia (one P-wave morphology and PR interval)
- multifocal atrial rhythm or wandering atrial pacemaker (rate < 100 bpm) or multifocal atrial tachycardia (rate > 100 bpm) (three or more different P-wave morphologies without any P-wave morphology being dominant)
- atrial fibrillation (no organized P waves).
No obvious atrial activity is seen in any lead. Hence this is atrial fibrillation with fine fibrillatory waves.
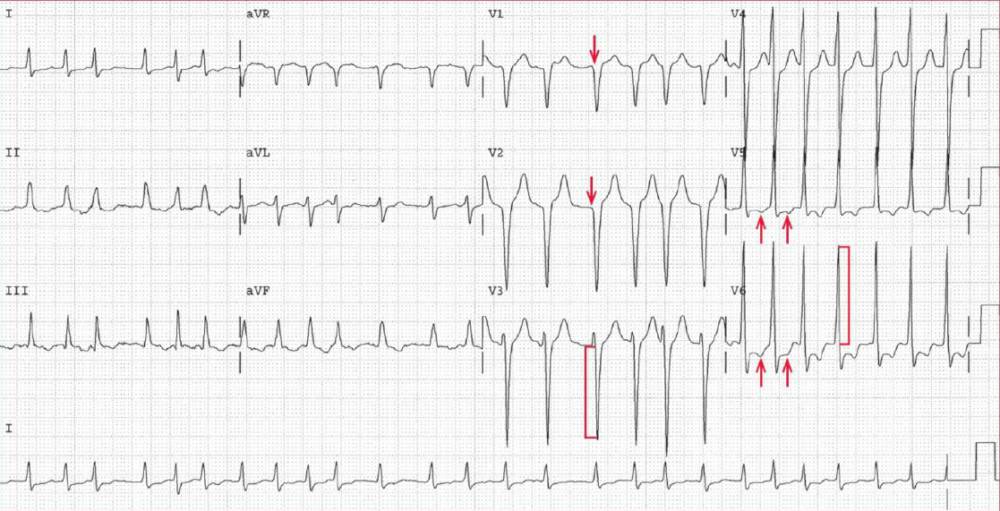
The amplitude of the QRS complex is increased (S-wave depth in lead V3 = 28 mm [ [ ] and R-wave amplitude in lead V6 = 25 mm [ ] ]; S-wave depth in lead V3 + R-wave amplitude in lead V6 = 53 mm), which is diagnostic for left ventricular hypertrophy (LVH). In addition, there are no R waves in leads V1-V2 (↓), suggesting an anteroseptal myocardial infarction, although this may also be the result of LVH.
ST-T wave abnormalities are noted in leads V5-V6 (↑); these are often associated with LVH. Although commonly called “strain,” they are actually repolarization abnormalities that result from chronic subendocardial ischemia.
These abnormalities are often seen with hypertrophy as the blood flow to the subendocardium (the last part of the myocardium to receive blood and oxygen supply) is reduced as a result of the hypertrophied myocardium as well as an increased left ventricular end-diastolic pressure that often occurs with hypertrophy.
Immediate therapy should be aimed at reducing the ventricular response rate. Rapid rate control can be achieved with AV nodal blocking agents such as beta-blockers and calcium-channel blockers. Digoxin also blocks the AV node by enhancing vagal tone.
- READ MORE:
- SIMILAR CASES: