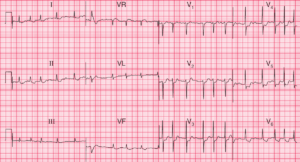
ECG Interpretation
- Regular broad complex tachycardia at about 230–240/min
- No P waves visible
- Right axis deviation
- QRS complex duration of about 180 ms
- QRS complexes point upwards in lead V1 and downwards in lead V6 – no concordance
- QRS complex configuration characteristic of right bundle branch block – but in lead V1 the first R wave peak is higher than the second peak
Clinical Interpretation
There are essentially three causes of a broad complex tachycardia: ventricular tachycardia, supraventricular tachycardia with bundle branch block, and the Wolff– Parkinson–White (WPW) syndrome.
The key to the diagnosis lies in the ECG when the heart is in sinus rhythm, but this is not always available. Patients with a broad complex tachycardia in the context of an acute myocardial infarction must be assumed to have a ventricular tachycardia, but that does not apply here.
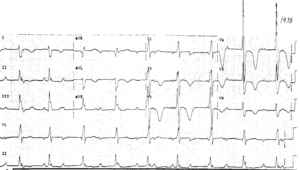
In this record the QRS complexes are not very broad, the axis is to the right, and there is no concordance of the QRS complexes – all pointing to a supraventricular origin.
In favour of a ventricular tachycardia is the fact that the height of the primary R wave in lead V1 is greater than that of the secondary R wave. However, taking these features together with the clinical picture, the rhythm is probably supraventricular.
What to do ?
Carotid sinus pressure and/or Valsalva maneuver is the first move. If there is severe haemodynamic compromise the patient may need urgent electrical cardioversion. Medications used to terminate symptomatic AVRT episodes and to reduce occurrences include b-blockers, calcium channel blockers, and antiarrhythmic drugs.
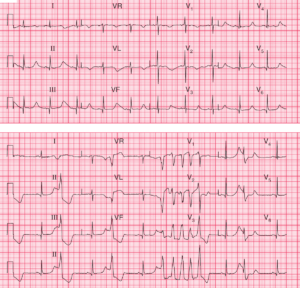
In fact, in this case the arrhythmia terminated spontaneously, revealing a short PR interval and a QRS complex with a delta wave. So this patient had the WPW syndrome, and needed an electrophysiological study with a view to ablation of the accessory tract.