This article is an answer to the ECG Case 161
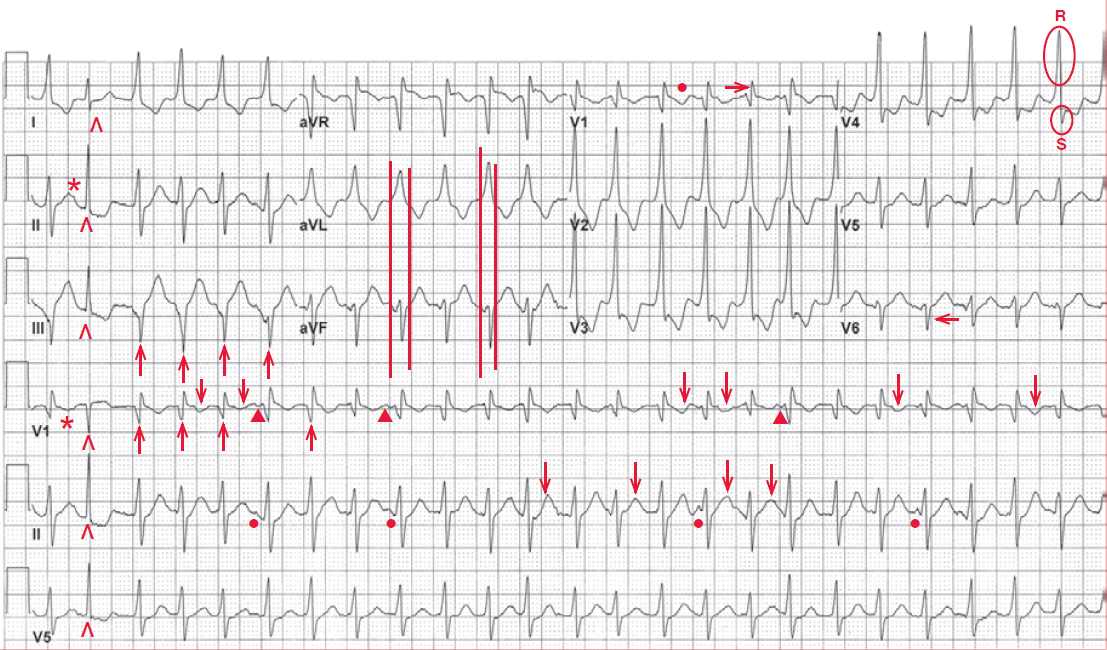
The ECG shows a regular rhythm at a rate of 148 bpm. The QRS complexes are wide, with a duration of 0.14 second. Although the QRS complexes resemble a right bundle branch block with an R wave in lead V1 (→) and a narrow S wave in lead V6 (←), there is no S wave in lead I and the morphology is not typical for a right bundle branch block. In addition it does not have a morphology of a left bundle branch block.
The axis is leftward, approximately –30° (QRS complex positive in lead I, negative in lead aVF and biphasic in lead II). There is one narrow QRS complex noted (0.08 sec) (^). Before this QRS complex there is a P wave present, best seen in lead II and the V1 rhythm strip (*); the PR interval is 0.18 sec.
There are other P waves seen (●, ▼), but none of them have a constant relationship to the QRS complexes, ie, they are dissociated. These P waves are most obviously seen in leads V1 and II rhythm strips, for example before the sixth, ninth, sixteenth, twenty-first QRS complexes (▼) in lead V1 and before the sixth, ninth, eighteenth complex in lead II (●).
In addition there are subtle differences in the ST-T wave morphologies (↓) (which represent either superimposed P waves or changes in repolarization). There are also subtle differences in QRS complex morphology (↑). Therefore, this wide complex tachycardia has AV dissociation, which is characteristic of ventricular tachycardia.
The narrow complex (^) is a captured or Dressler beat, which is a feature of AV dissociation. The subtle differences in ST-T waves and QRS complex morphology are characteristic of ventricular tachycardia. This is due to the fact that ventricular activation does not occur via the normal Purkinje pathway, but rather is directly through the ventricular muscle. Therefore, there may be changes in the activation and repolarization sequence due to local characteristics of the ventricular myocardium, resulting in the QRS and ST-T wave changes.
In contract, each QRS complex of a supraventricular tachycardia, regardless of where it originates (sinus node, atrial myocardium, or AV node) is always conducted to the ventricles via the same pathway (ie, His-Purkinje or accessory pathway) and hence the activation and repolarization sequence is always the same for each complex.
Lastly, there are RS complexes in leads V4–V6 and the R wave is wider than the S wave, reflecting abnormal conduction of the initial portion of ventricular activation—another feature of a ventricular complex.
It should be noted that the small negative waveforms noted before the QRS complex in lead aVF are actually part of the QRS complex if the maximum QRS duration as noted in lead aVL is compared to the QRS complex in lead aVF (║).
The QRS morphology of the ventricular tachycardia resembles a right bundle branch block and has a leftward axis (borderline for a left anterior fascicular block). In addition the QRS complex is not extremely wide. These features are consistent with a fascicular tachycardia, ie, involving one of the fascicles of the left bundle. In this case, it would be a left posterior fascicular tachycardia, resulting in the QRS morphology and axis noted.
A left posterior fascicular tachycardia is the most common type of fascicular tachycardia. A fascicular tachycardia, which is a type of idiopathic left ventricular tachycardia, is also called verapamil-responsive ventricular tachycardia or Belhassen tachycardia. It is commonly seen in younger patients without heart disease and it is not usually associated with a risk of sudden cardiac death, as there is often no structural heart disease present.