This article is an answer to the ECG Case 179
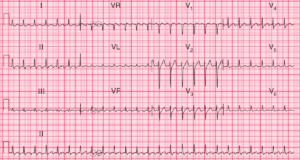
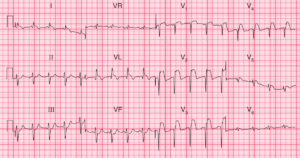
There is a regular rhythm at a rate of 100 bpm, with a P wave (*) before each QRS complex and a stable PR interval (0.16 sec). The P wave is upright in leads II, aVF, and V4-V6 and negative in lead aVR. This is a sinus tachycardia.
The QRS complex duration (0.08 sec) and morphology are normal. The QRS axis is not able to be determined accurately because of very significant ST-segment elevation (↓) in leads II, III, and aVF. ST-segment elevation (↓) can also be seen in lead V6. The ST segments are convex and are merged with the T waves.
There is also ST-segment depression (^) in leads I, aVL, and V2-V4. The ECG is typical for an acute inferior wall ST-segment elevation myocardial infarction (STEMI), and the ST-segment depressions are reciprocal changes, although in leads V2-V3 the depressions represent involvement of the posterior wall of the left ventricle.
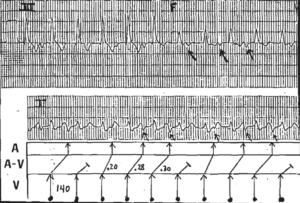
Interestingly, there is evidence of ST-segment alternans (ie, beat-to-beat changes in the height of the ST segment), best seen in leads aVL and aVF. This has primarily been described with coronary artery vasospasm and transient occlusion of a coronary artery during angioplasty. It is a marker of more severe transmural ischemia.