This article is an answer to the Case – Liver Failure, Ascites, and Absent Right-Sided Breath Sounds
Radiologic Findings
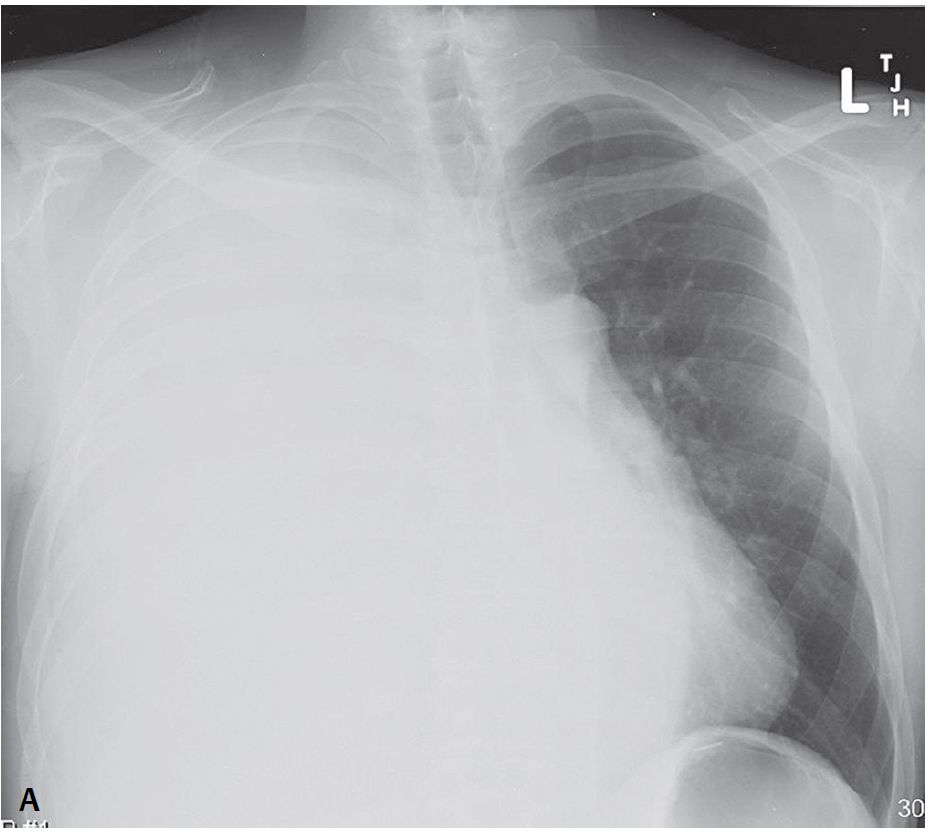
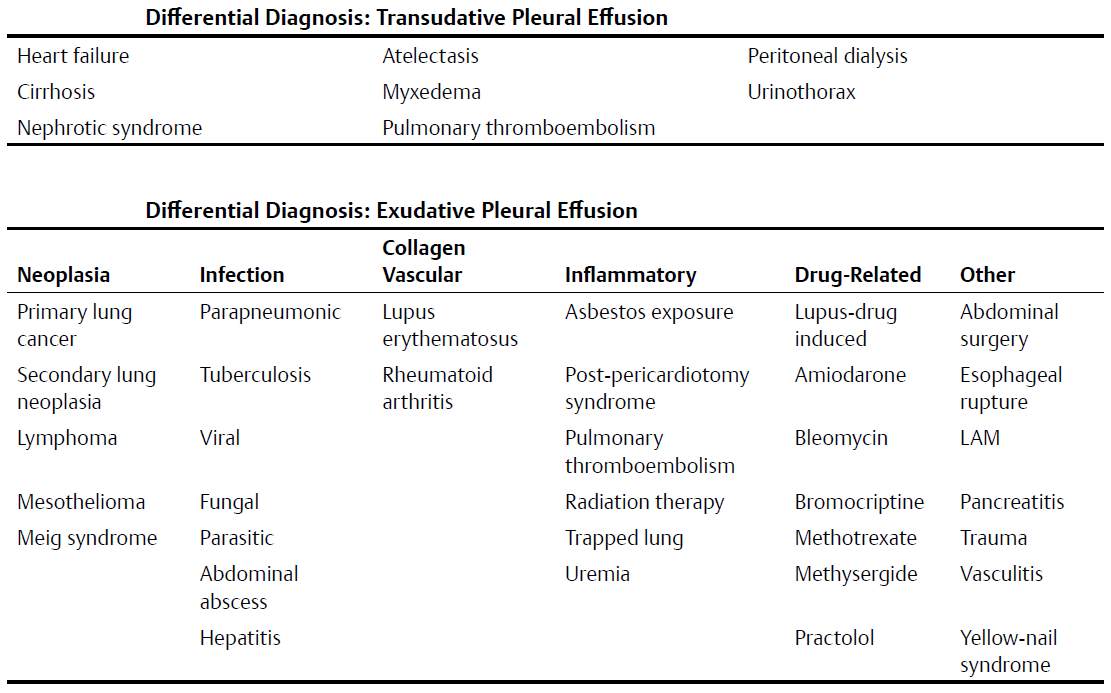
PA chest radiograph show complete “white-out” of the right hemithorax. No air bronchograms are seen and only the left diaphragm is perceptible on the lateral exam. Note the contralateral displacement of the tracheal air column and mediastinum “away” from the white-out on the PA exam.
Diagnosis
Massive Unilateral Pleural Effusion; Hepatic Hydrothorax
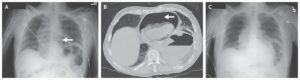
Differential Diagnosis
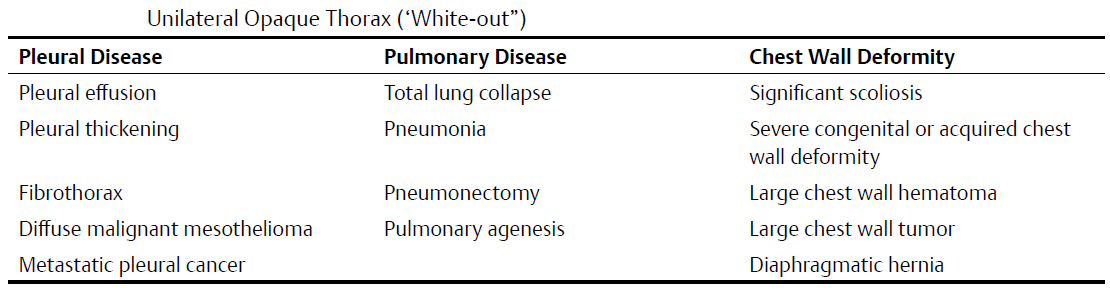
- Unilateral Opaque Thorax (“White-out”) is quite broad (see table bellow)
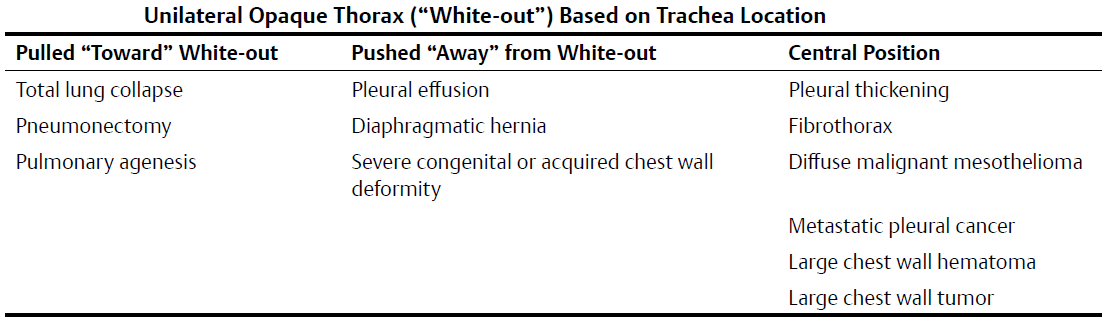
- Differential can be narrowed based on location of trachea (see table bellow)
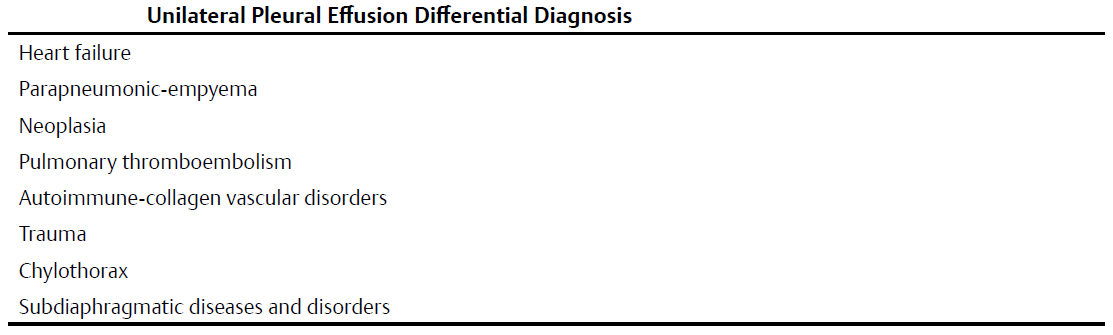
- Other Causes of Unilateral Pleural Effusion (see table bellow)
Etiology of Pleural Effusion
Thoracentesis is usually performed to evaluate pleural effusions of unknown etiology. Fluid is examined grossly and submitted for biochemical analysis, red and white blood cell counts, Gram and acid-fast stains, and cytology. More invasive procedures, including closed, open, or thoracoscopic biopsy, are sometimes necessary to establish a diagnosis.
Most effusions are categorized as transudates or exudates using criteria established by Light. Such categorization is useful in narrowing the differential diagnosis (see tables bellow) and dictating patient management.
Exudates exhibit one or more of the following characteristics:
- pleural fluid protein/serum protein ratio >0.5;
- pleural fluid lactic acid dehydrogenase (LDH)/serum LDH ratio >0.6;
- pleural fluid LDH ratio greater than two-thirds the normal serum LDH.
Transudates are characteristically clear, straw-colored, have a low protein concentration, and have few cells. Most transudates result from systemic factors that alter pleural fluid formation or absorption.
Exudative effusions result from diseases that alter the pleural surface and its permeability to protein. Bilateral pleural effusions sometimes have different etiologies (Contarini condition)—for example, an exudative pleural effusion (empyema) in one thorax and a transudative pleural effusion (heart failure) on the other side.
Pleural effusions may also be characterized by their composition (e.g., hydrothorax, hemothorax, pyothorax, chylothorax, bilothorax, urinothorax, pyohemochylothorax).
Clinical Findings
The clinical presentation varies depending on the underlying cause of the effusion and how rapidly the pleural fluid accumulated. Some patients are asymptomatic (15%), whereas others present with dull aching chest pain, cough, fever, and dyspnea. Large effusions may displace the mediastinum and cause respiratory distress. Physical exam findings may include decreased or absent breath sounds over the affected thorax and dullness to percussion.
Imaging Findings
Chest Radiography
- Hazy increase in radio-opacity (i.e., ground glass veil) that does not obscure underlying bronchovascular markings on supine chest radiography
- Radio-opacity involving posterior or lateral costophrenic sulcus with meniscus-shaped upper border (i.e., blunting) on upright radiography
- Smooth meniscus-shaped opacity, the upper border of which curves gently downward from its lateral aspect to the mid-cardiac region in small to moderate pleural effusions
Predicting Volume of Pleural Fluid
- Lateral decubitus exam: may demonstrate as little as 5 mL of pleural fluid; also useful in differentiating loculated from mobile pleural fluid collections
- Posterior costodiaphragmatic sulcus blunting on lateral chest radiography: 20–30 mL
- Lateral costodiaphragmatic sulcus blunting on frontal chest radiography: 200–300 mL
- Obscuration of ipsilateral hemidiaphragm on frontal radiography: >500 mL
Subpulmonic Pleural Effusion
- Bilateral subpulmonic effusions unlikely to be recognized; mimics hypoventilation
- Lateral displacement of apex of apparent diaphragm (i.e., pseudodiaphragm) on frontal exams
- Convex margin of fluid flattens as it contacts oblique fissure and descends abruptly to anterior costophrenic sulcus on lateral radiography; Rock of Gibraltar sign
- ± Small amount of fluid in inferior aspect of oblique fissure on lateral radiography
- Left-sided effusion may be characterized by downward displacement of gastric air bubble from pseudodiaphragm by ≥2.0 cm on upright chest exams
Interlobar Fluid Collections (Pseudotumor; Vanishing Tumor)
- Most often associated with heart failure; renal failure and hepatic hydrothorax less often
- Invariably radiographic evidence of concomitant or resolving heart failure
- Homogeneous ovoid opacity oriented along long axis of fissure
- Evidence of ipsilateral pleural fluid
- Absence of air bronchograms
- Morphology changes from one orthogonal view to the next
- Mobile with decubitus positioning
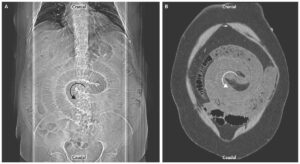
MDCT
- Sensitive in detection of free pleural fluid
- Layers posteriorly with characteristic meniscoid appearance
- Attenuation coefficients: 0–20 HU; higher with hemothorax
- Small effusions may be difficult to differentiate from pleural thickening; fibrosis; dependent atelectasis; decubitus CT imaging aids in differentiation
- Dependent lung may appear to “float” in the fluid of large effusions
- Loculated effusion: sharply marginated lenticular fluid attenuation mass; conforms to concavity of chest wall; forms obtuse margins at its edges; compresses adjacent lung
- Septations indicative of complicated, organizing effusion
- Pleural fluid and ascites may occur concurrently; relationship to diaphragm, bare area of liver, and interface with liver and spleen aid in differentiation
Ultrasound
- Effusions displace lung away from chest wall; allows visualization of pleural cavity
- Most pleural fluid is anechoic or hypoechoic (e.g., transudate, exudate); may see floating particulate matter
- Septations not apparent on CT are often evident; septations, floating particles or layering debris, increased echogenicity more suggestive of exudate
- Collapsed/consolidated lung moves within the effusion during respiration
MRI
- Signal intensity of pleural fluid depends on its biochemical characteristics
- Most cases of non-hemorrhagic or non-chylous effusion:
- High signal intensity: T2WI
- Low signal intensity: T1WI
Management
Transudative Effusion
- Systemic disorder is treated; no further investigation is necessary
Exudative Effusion
- Further investigation is warranted to determine its etiology and is then directed toward that disease process
Prognosis
Dependent upon the underlying disease process
Pearls
- Heart failure is the most common cause of transudative pleural effusion encountered in clinical practice.
- Parapneumonic effusion is the most common cause of exudative pleural effusion; neoplasia is the second most common cause.
- Interlobar pseudotumor: interlobar accumulation of interfissural fluid that can mimic but should be differentiated from a true lung mass. Although this may occur in any standard or accessory fissure, there is a predilection for it to occur in the horizontal fissure. Remember that these fluid collections are “localized” and not “loculated” within the fissure and will easily layer out on decubitus exams.
- The majority of massive unilateral pleural effusions are malignant (e.g., primary lung cancer, metastatic disease, lymphoma).
Suggested Reading
- Falaschi F, Battolla L, Mascalchi M, et al. Usefulness of MR signal intensity in distinguishing benign from malignant pleural disease. AJR Am J Roentgenol 1996;166(4):963–968
- Halvorsen RA, Fedyshin PJ, Korobkin M, Foster WL Jr, Thompson WM. Ascites or pleural effusion? CT differentiation: four useful criteria. Radiographics 1986;6(1):135–149
- Hierholzer J, Luo L, Bittner RC, et al. MRI and CT in the differential diagnosis of pleural disease. Chest 2000;118(3): 604–609
- Light RW. Clinical practice. Pleural effusion. N Engl J Med 2002;346(25):1971–1977
- Travis WD, Colby TV, Koss MN, Rosado-de-Christenson ML, Muller NL, King TE Jr. Pleural disorders. In: King DW, ed. Atlas of Nontumor Pathology: Non-Neoplastic Disorders of the Lower Respiratory Tract, first series, fascicle 2. Washington, DC: American Registry of Pathology; 2002:901–921