This article is an answer to the Case – Patient with Symptoms of Eye and Ear Pain
Examination revealed bilateral erythema and tenderness of the auricles and thickening and deformity of the pinnae with sparing of the ear lobules and no joint abnormalities. The right tympanic membrane was congested.
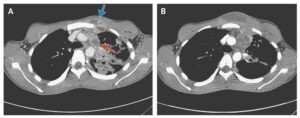
Ophthalmologic examination revealed bilateral congestion and inflammation of the conjunctival, episcleral, and scleral vessels. The congested area did not blanch with the instillation of phenylephrine eyedrops — a finding that is consistent with a diagnosis of scleritis. Posterior scleritis was identified by the presence of bilateral optic-disk edema and hyperemia on slit-lamp examination and by the presence of a thickened sclera on ultrasonography.
The diagnosis of Polychondritis was made. Polychondritis is a systemic autoimmune disease involving the cartilaginous tissues of the face, joints, and the respiratory tract. There is intermittent inflammation that can present with swelling in the ears, eye pain, cough, wheezing, and joint swelling. Up to 30% of patients have co-existing autoimmune diseases. The treatment of polychondritis often includes NSAIDs, steroids, or other forms of immunosuppressive therapy depending on the severity of the disease.
Laboratory workup was unrevealing. The patient was treated with prednisone, topical glucocorticoids, and cycloplegic eyedrops, with a good response.