Table of Contents
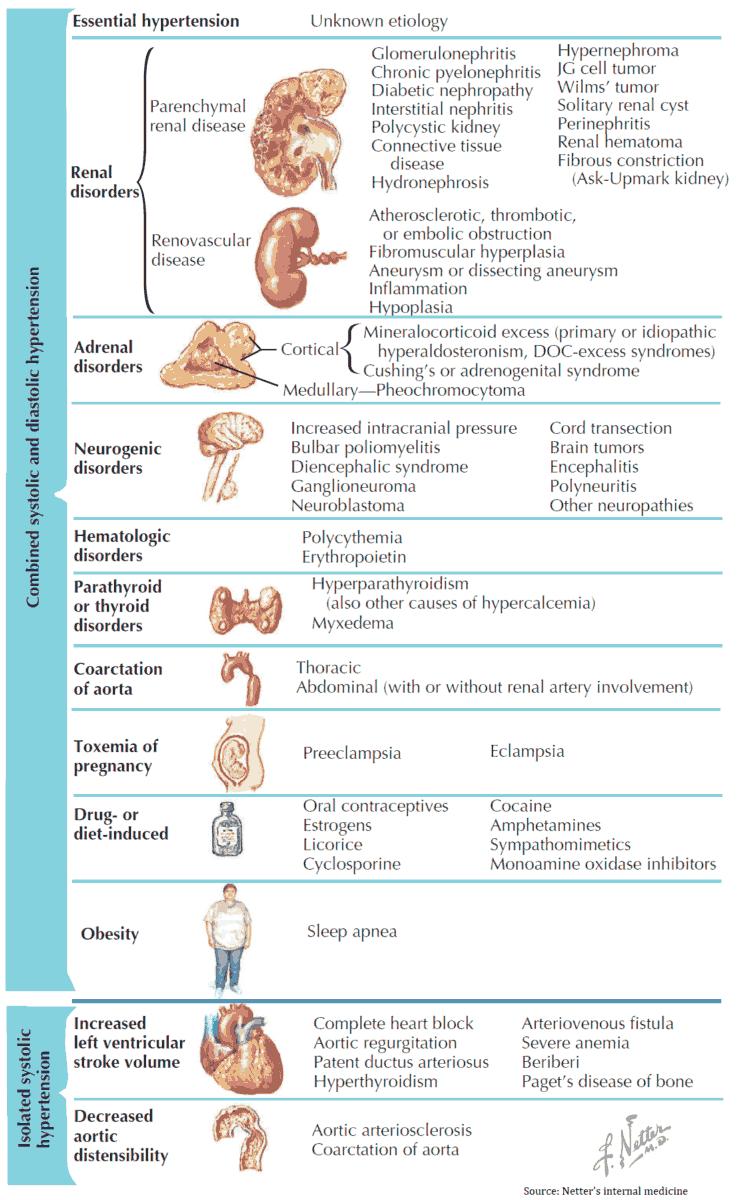
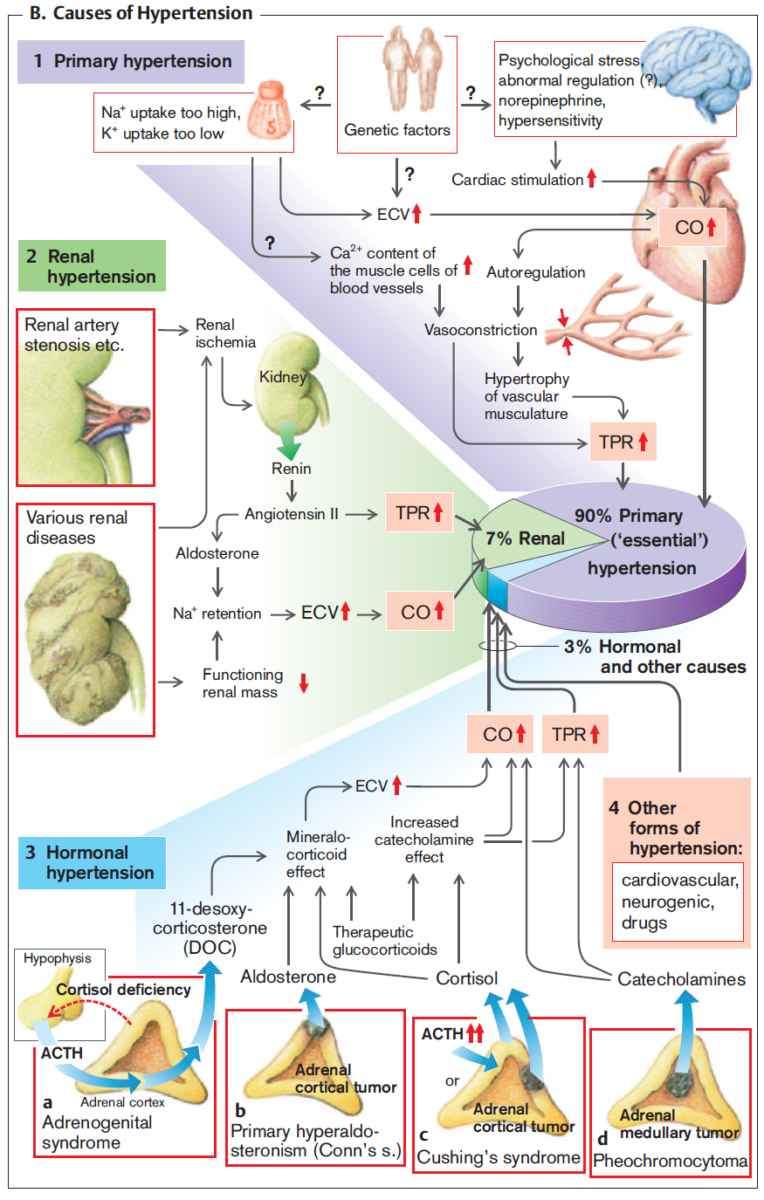
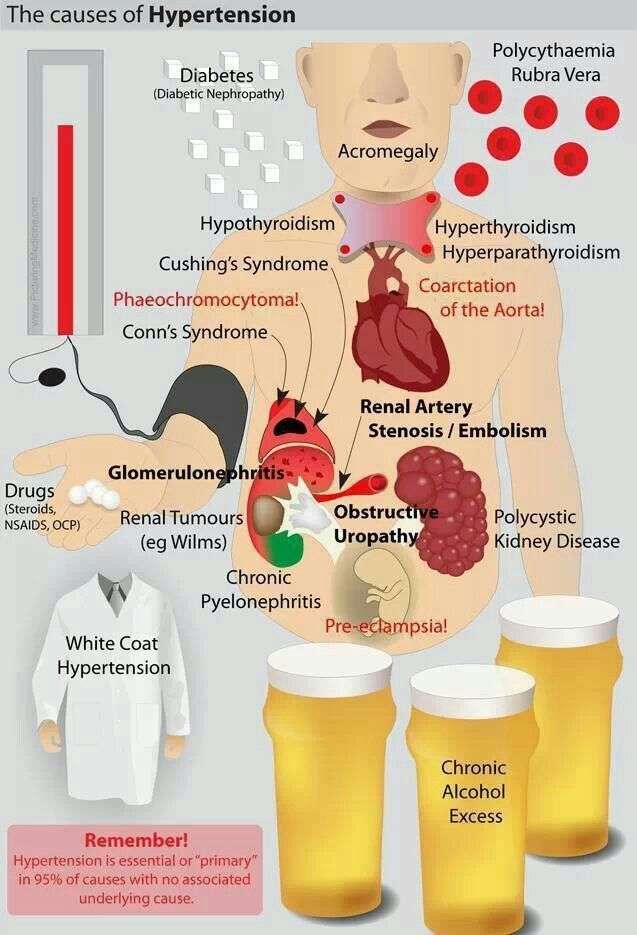
Approximately 95% of all hypertensive patients have “essential” or “primary” hypertension and have no underlying disease. Secondary hypertension can be the result of a range of different pathologic processes.
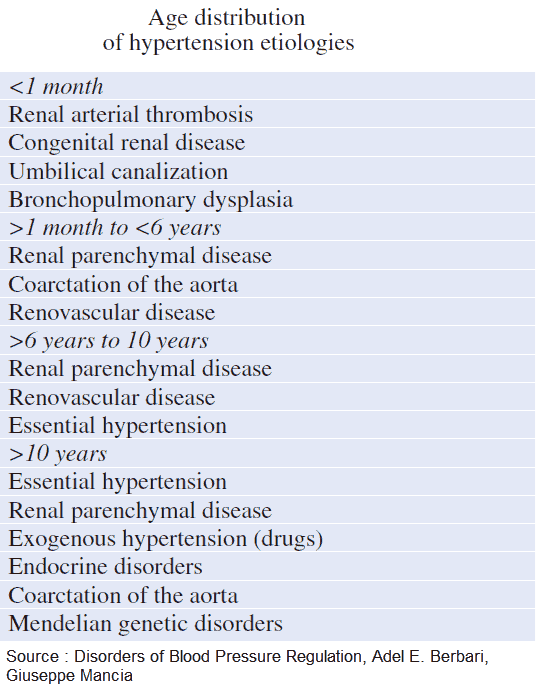
Hypertension is present in 20-30% of the population, depending on ethnic background. African-Americans have higher blood pressures than Hispanic and Caucasian populations. The incidence increases with age; hypertension is present in 55-80% of the population over the age of 60 years.
Causes and Differential Diagnosis of Hypertension
Essential Hypertension
Essential hypertension accounts for 95% of cases. There is no underlying cause.
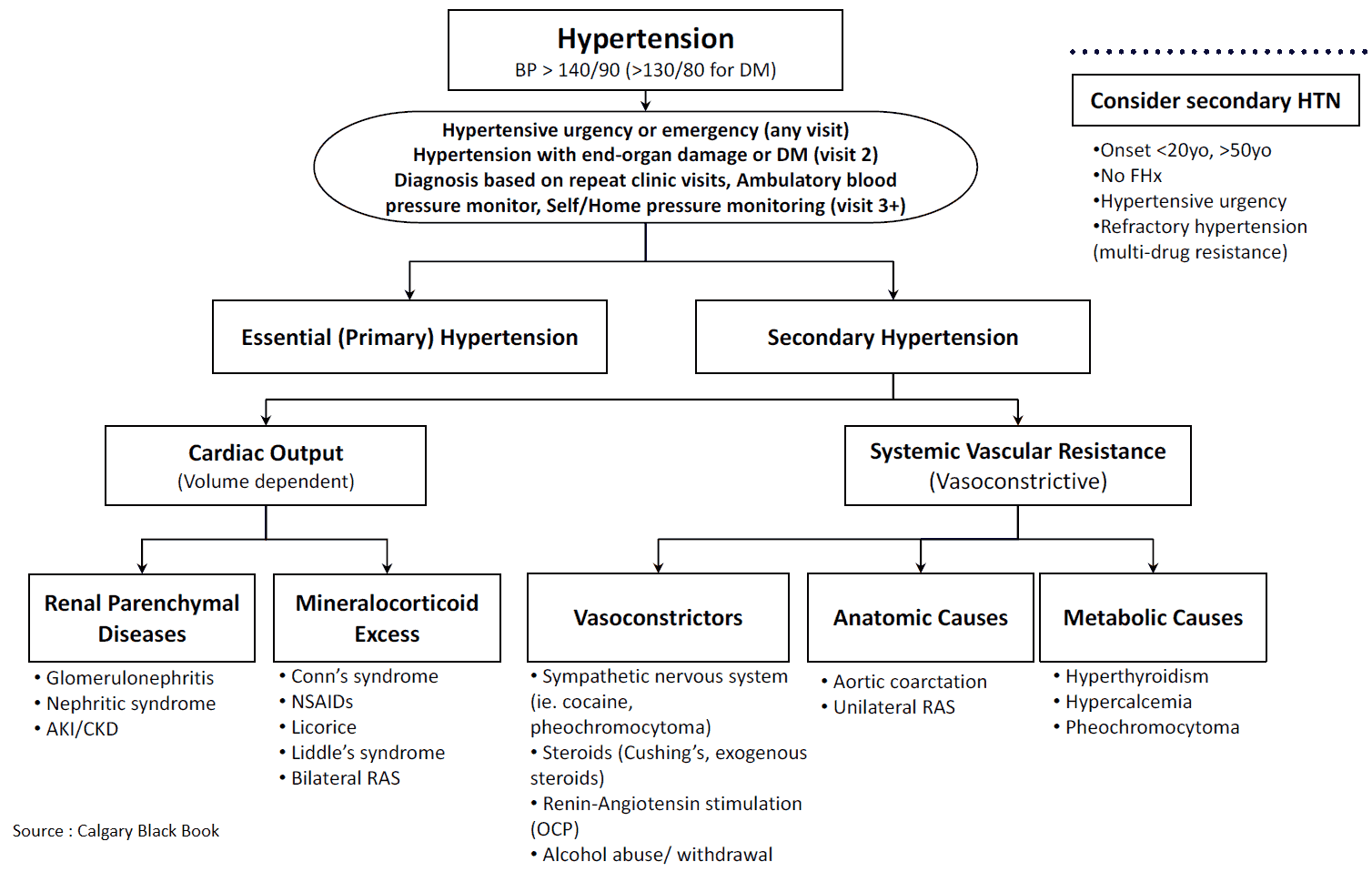
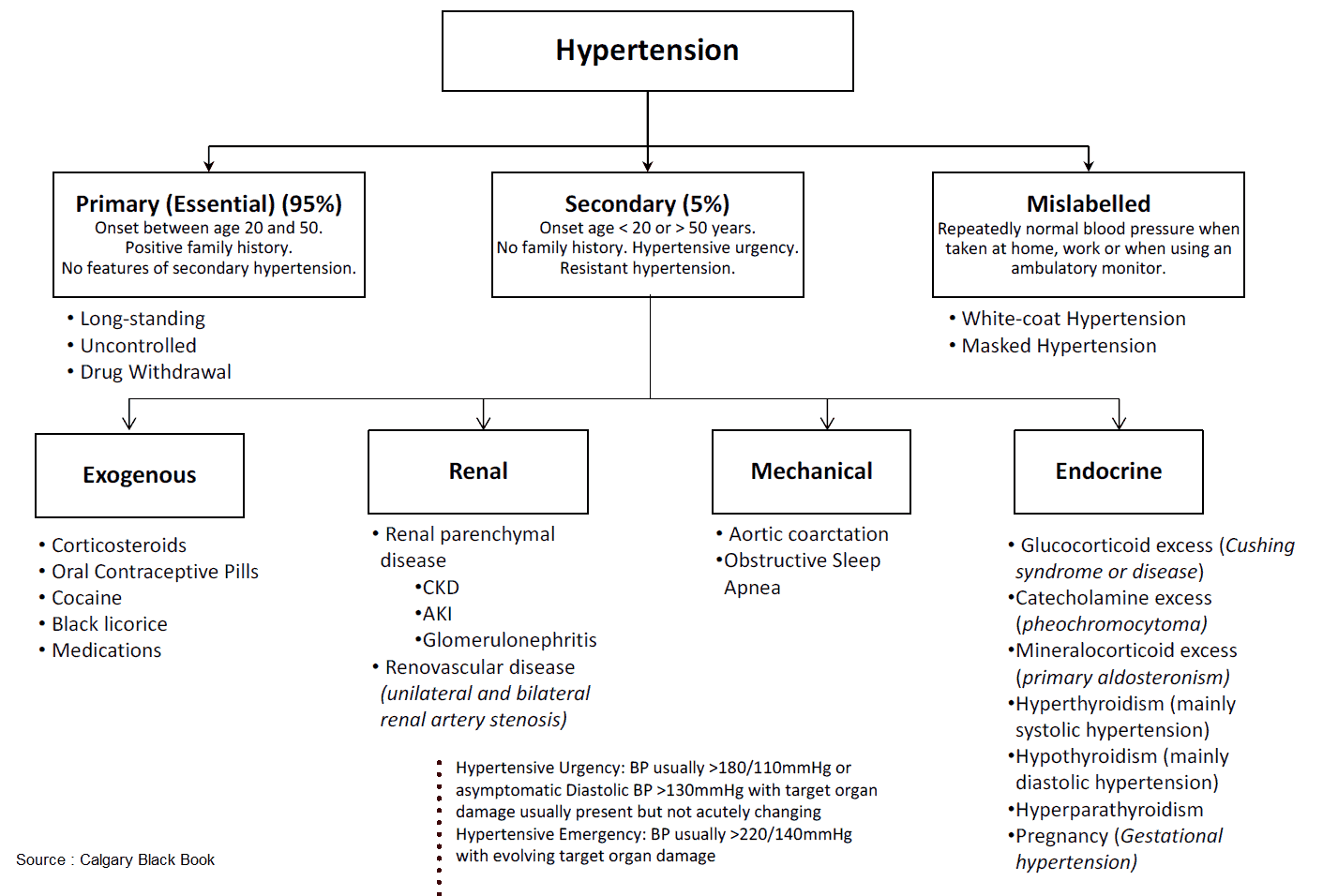
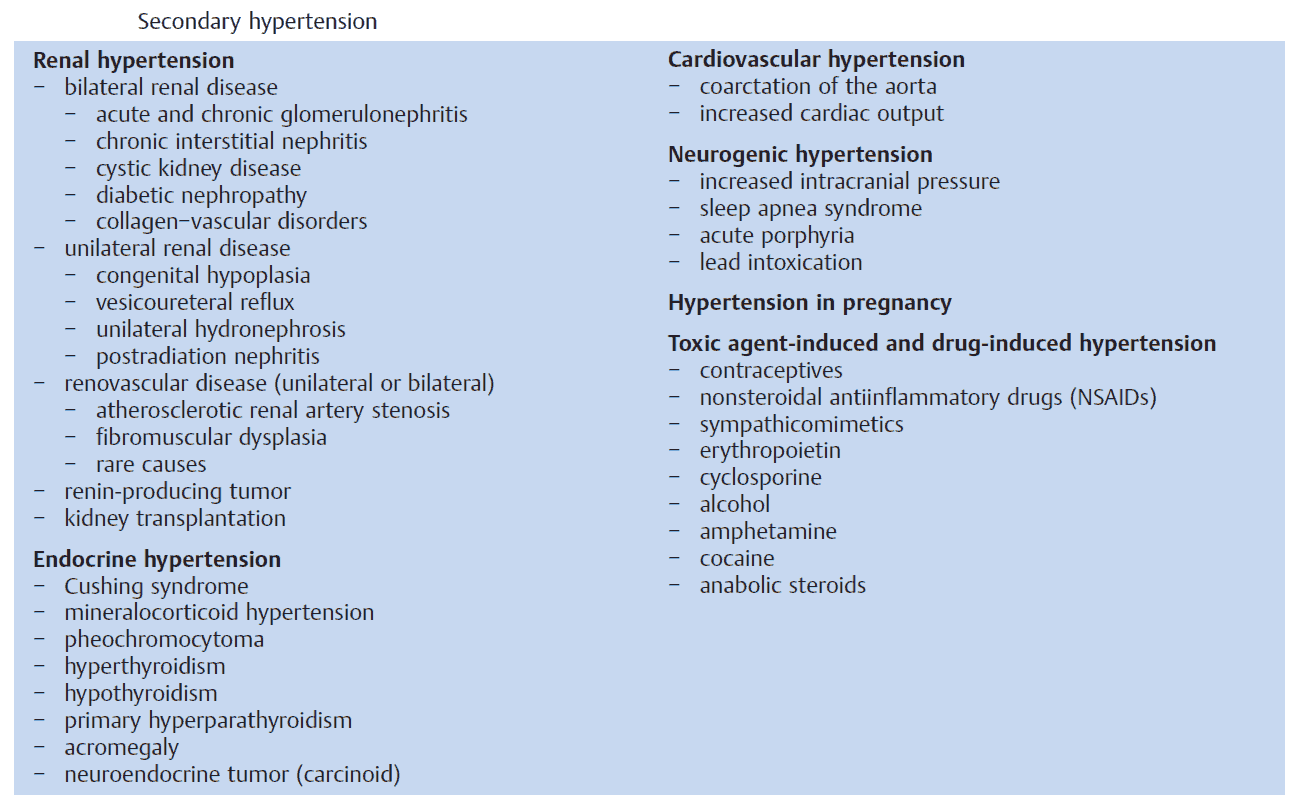
Secondary Hypertension
Secondary hypertension accounts for 5% of cases. Factors leading to secondary hypertension are:
Lifestyle
- Obesity.
- High alcohol intake.
- Lack of exercise.
- High salt intake.
Renal
- Renal parenchynmal disease (e.g., chronic pyelonephritis, glomerulonephritis, polycystic disease, tumor, tuberclosis).
- Renal artery disease (e.g., atherosclerosis, fibromuscular dysplasia, vasculitis).
- Obstructive uropathy (e.g., hydronephrosis due to a stone or tumor).
Cardiovascular
- Congenital (e.g., coarctation of the aorta).
Drugs
Examples include:
- Combined oral contraceptive pill.
- Nonsteroidal anti-inflamatory drugs [NSAIDs]).
Endocrine
- Pheochromocytoma.
- Conn’s syndrome.
- Secondary hyperaldosteronism.
- Cushing’s syndrome.
- Hyperthyroidism.
- Hypercalcemia.
- Obesity.
Other
- Raised intracranial pressure.
- Obstructive sleep apnea.
History in the patient with hypertension
Hypertension is usually asymptomatic and is often found incidentally. The history should be approached in three parts:
- Firstly, how long has the patient had hypertension and what treatments have been given so far?
- Secondly, how severe is the hypertension and has it resulted in complications?
- Finally, are there any risk factors suggesting that an underlying pathology may be present?
Presentation and history of hypertension
Important questions to address are as follows:
- How was the hypertension discovered? For example, at a routine preoperative assessment or with malignant (accelerated) hypertension. When was the last time that the patient had a normal blood pressure reading?
- For how long has the blood pressure been monitored? Unless severe (>160/100 mmHg), the diagnosis should not be made until blood pressure is persistently elevated for at least 6 months.
- What treatments, if any, has the patient been given so far? If blood pressure control is poor, despite taking correct doses of three antihypertensive agents, the patient is said to have “resistant hypertension.”
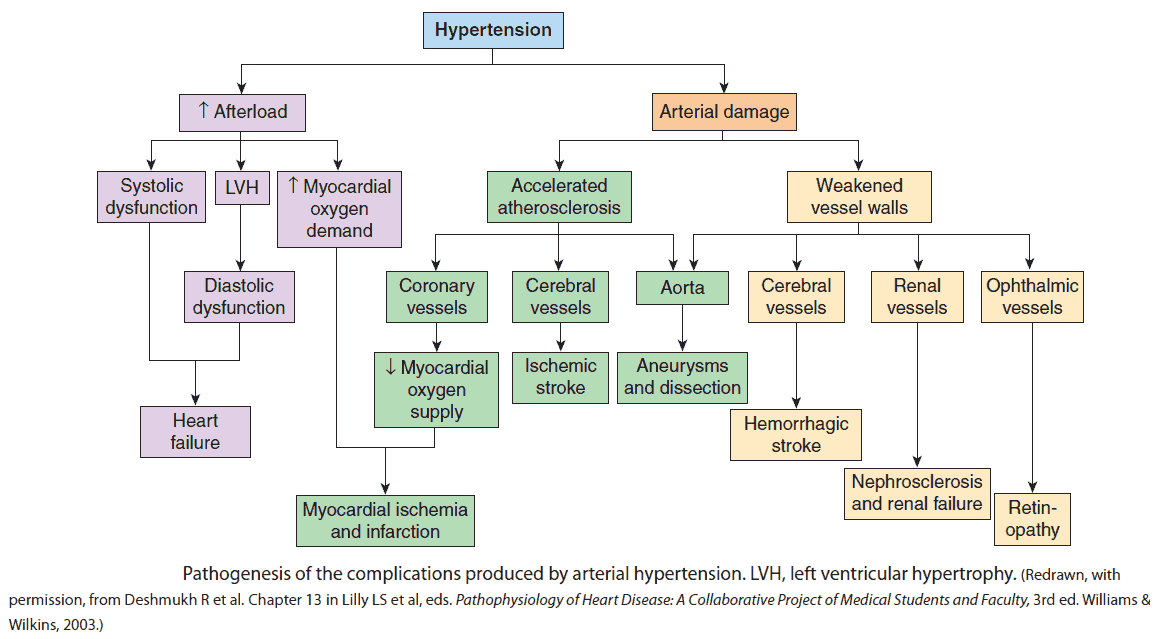
How severe is the hypertension? Are there complications?
Mild hypertension is asymptomatic. However, when hypertension is severe or chronic and associated with complications, the following symptoms may occur:
- Headaches (mostly frontal).
- Dyspnea.
- Symptoms of frank heart failure.
- Angina pectoris or myocardial infarction.
- Transient ischemic attacks or stroke.
- Visual disturbance.
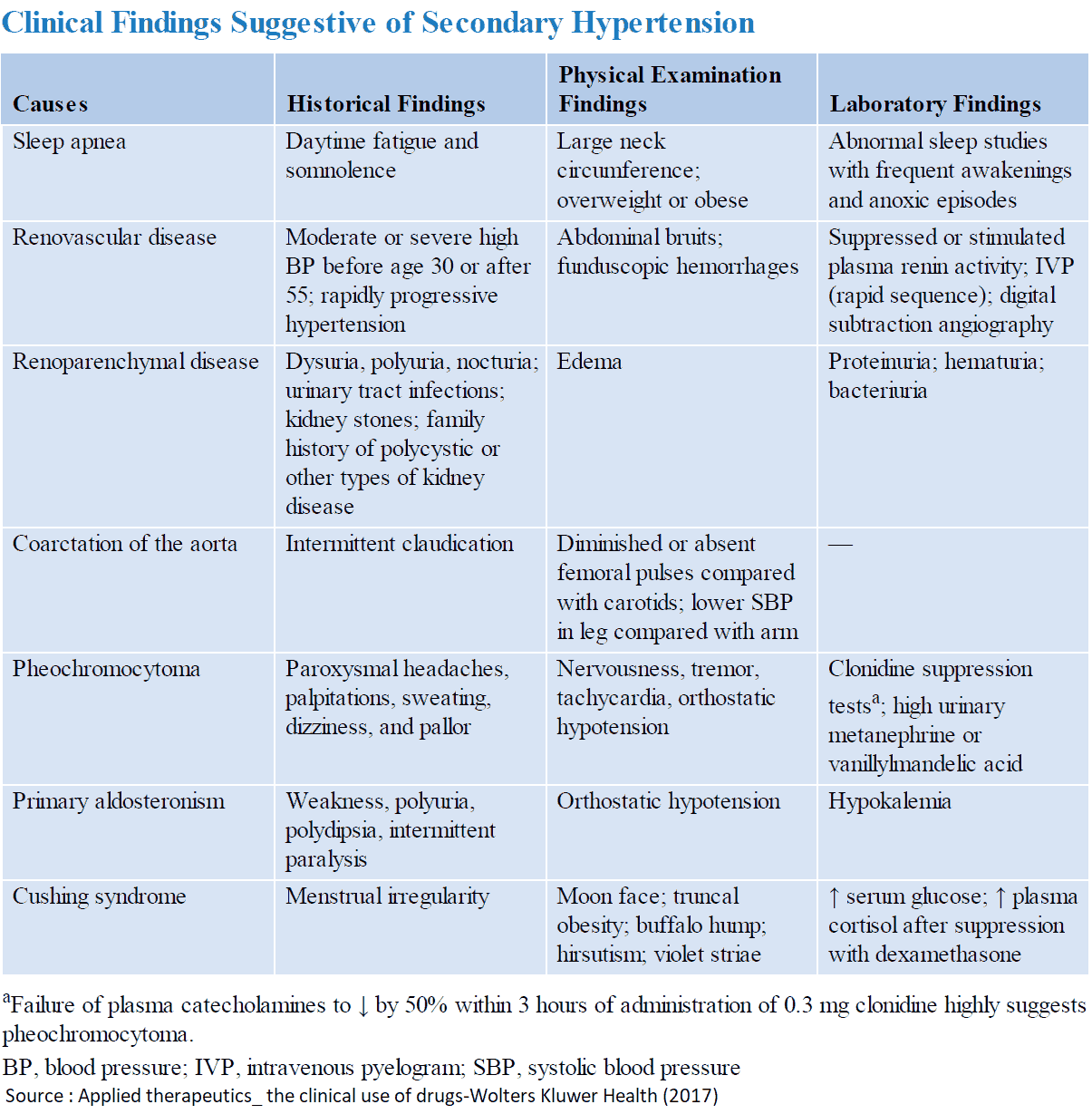
Is the history suggestive of an underlying cause?
Ask about the following:
- Lifestyle history, paying particular attention to alcohol and smoking (atherosclerosis). Stimulants such as cocaine and amphetamines can also cause hypertension.
- Precise drug history.
- Previous medical history (e.g., recurrent pyelonephritis, nephrectomy).
- Family history may suggest underlying polycystic disease.
- Symptoms of pheochromocytoma are rare but include episodic pallor, headache, tremor, palpitations, and nausea.
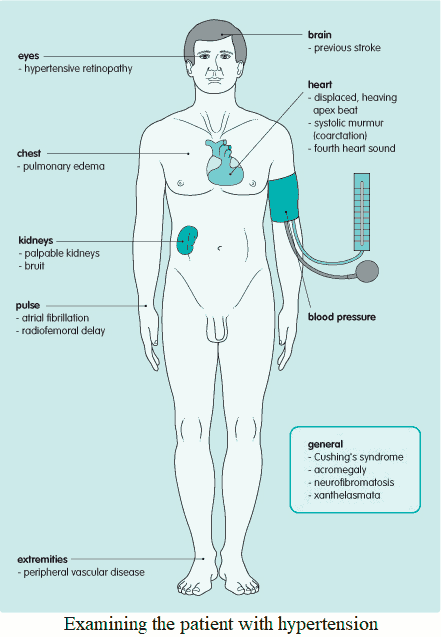
Examining the patient with hypertension
Patients with uncomplicated mild essential hypertension will have no associated clinical signs. However, when a patient is found to be hypertensive, one should search for evidence of complications or an underlying cause.
Evidence of an underlying cause
- Palpable kidneys: polycystic disease, renal tumor.
- Peripheral vascular disease and xanthelasmata: renal artery stenosis.
- Renal bruit (throughout both systole and diastole): renovascular disease.
- Radiofemoral delay: coarctation of the aorta.
- Neurofibromatosis: renal artery stenosis.
- Cushing’s disease.
Evidence of complications
- Atrial fibrillation.
- Displaced, thrusting PMI, indicating left ventricular hypertrophy.
- Frank heart failure.
- Retinopathy.
- Previous stroke.
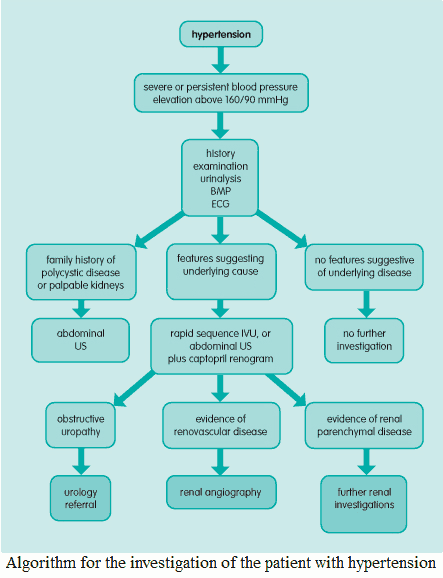
Investigating the patient with hypertension
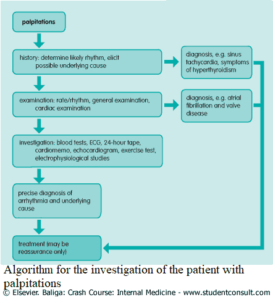
At presentation all hypertensive patients should have the following tests:
- Urine dipstick: parenchymal disease, urinary tract infection, stone, associated diabetes.
- Metabolic panel: renal impairment suggests underlying disease.
- Lipid profile: to rule out metabolic syndrome.
- Electrocardiogram: significant hypertension may result in left ventricular hypertrophy (LVH).
- Echocardiogram. Most patients have an echocardiogram to look for LVH. While the ECG is helpful, an echocardiogram can give information not only about LVH but also about any wall motion abnormalities.
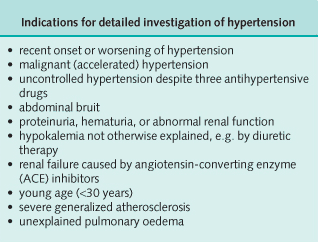
Patients diagnosed with hypertension at an early age and patient initially resistant to multiple antihypertension medication should be investigated further. The following tests may be used:
- 24-hour urinary vanilly mandelic acid (VMA) and catecholamine excretion: pheochromocytoma.
- Radiologic investigations: renovascular disease, renoparenchymal disease, obstructive uropathy. This should be either rapid sequence intravenous urogram, or abdominal ultrasound scan plus captopril renogram.
- Renal angiography: renal artery disease; this is a definitive test and should be performed if indicated by the radiologic tests or clinical circumstances.