Table of Contents
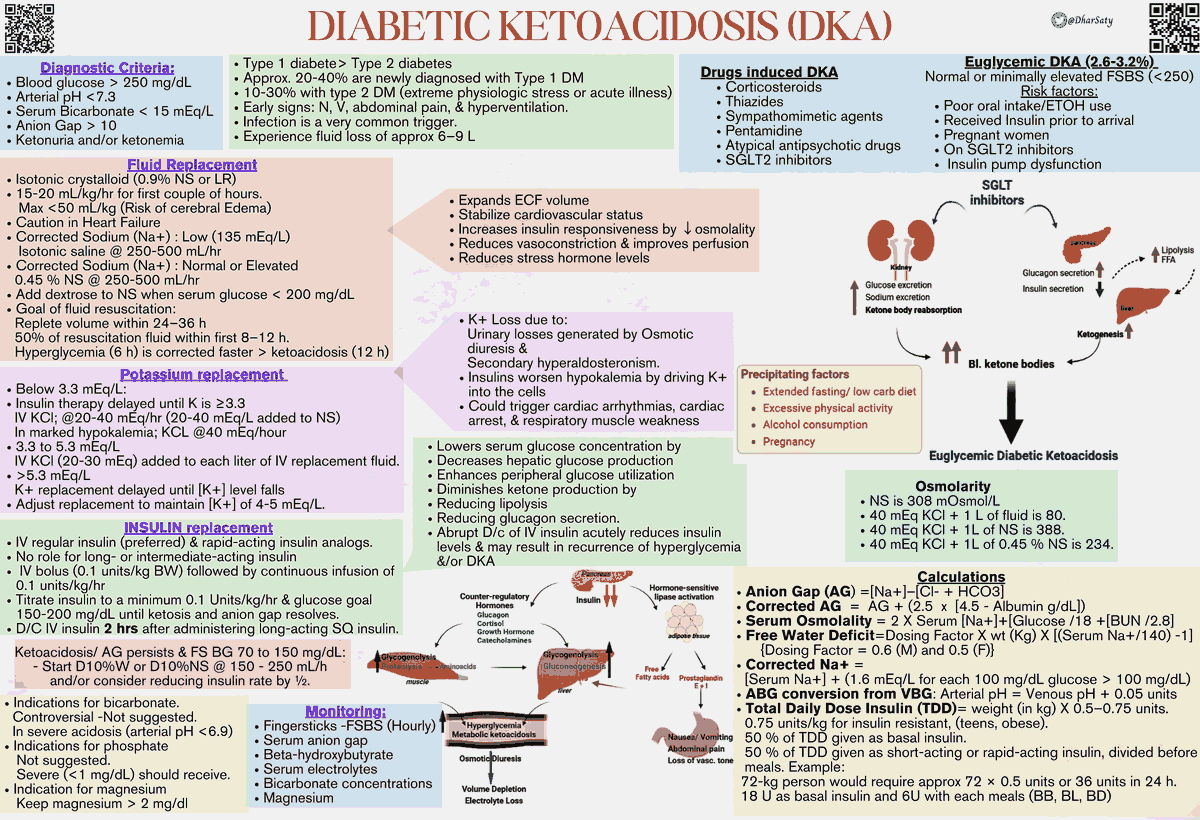
Diabetic ketoacidosis (DKA) is a critical metabolic derangement that is commonly precipitated by acute illness (i.e., infection, myocardial infarction, stroke) or medication noncompliance.
The American Diabetic Association and the International Society for Pediatric and Adolescent Diabetes provide clinical guidelines for the management of patients with DKA. Notwithstanding, these guidelines are complex and can be difficult to follow.
Given the mortality associated with DKA, it is imperative for the emergency provider (EP) to be knowledgeable on several pitfalls that can occur in the emergency department management of these critically ill patients.
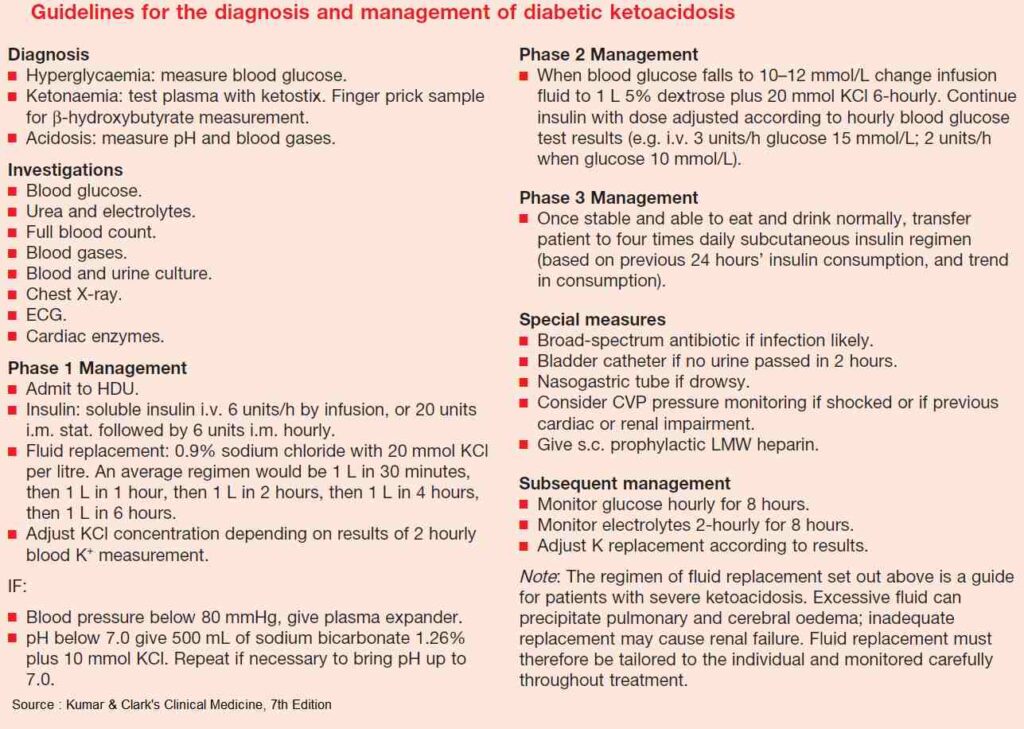
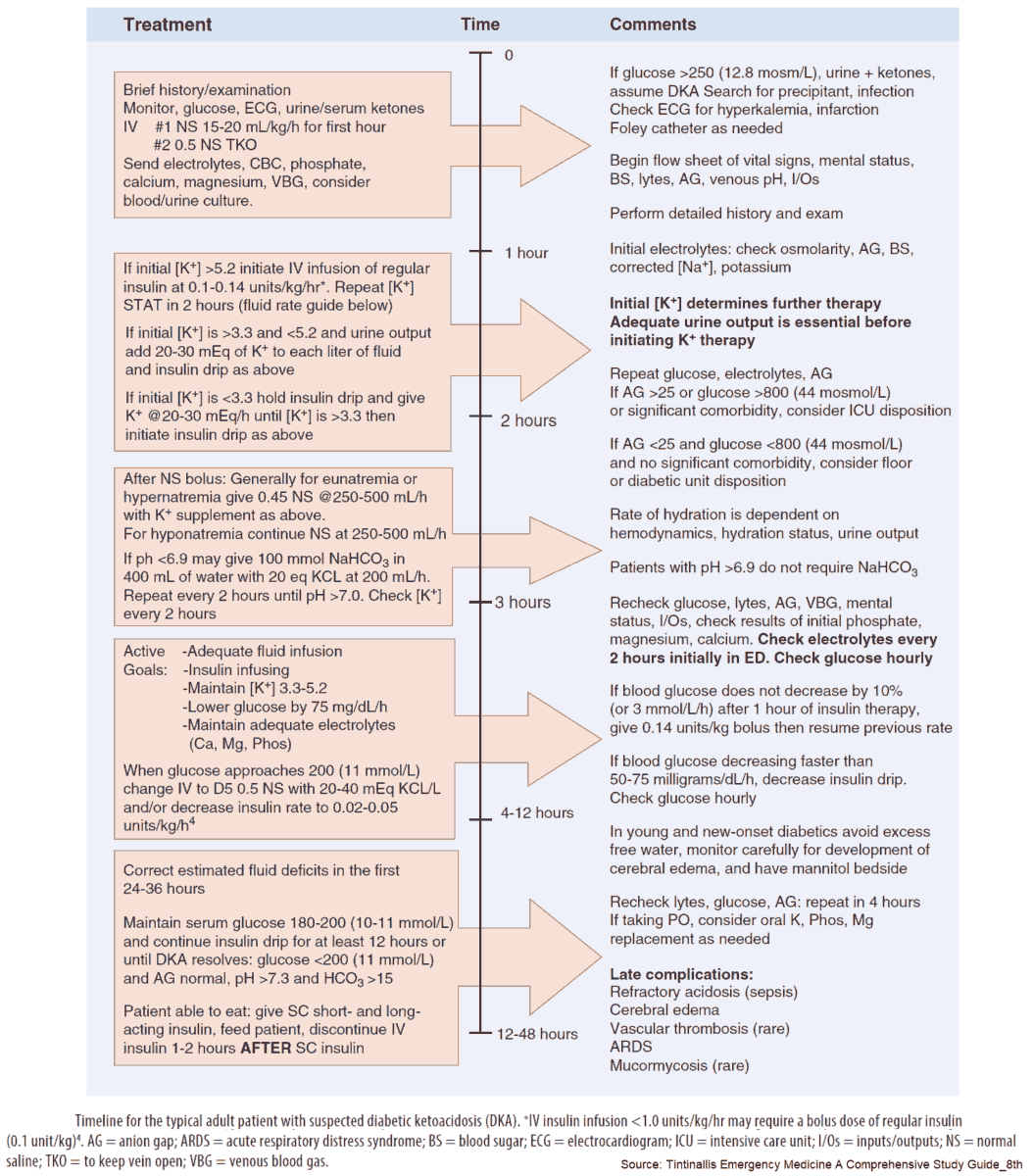
Intravenous Fluids
Initial management of the DKA patient should begin with intravenous fluid administration. Current guidelines recommend an initial bolus of 15 to 20 mL/kg of 0.9% normal saline. It is important to note that 0.9% normal saline contains supraphysiologic concentrations of chloride.
Hyperchloremia is believed to be an inflammatory stimulus and is associated with adverse effects on the renal, pulmonary, cardiovascular, and splanchnic organ systems. Moreover, the strong ion difference of 0.9% normal saline is zero. Thus, 0.9% normal saline will reliably induce a hyperchloremic metabolic acidosis and potentially worsen the already disturbed acid-base balance in patients with DKA.
Recently, balanced solutions (i.e., Plasma-Lyte) have been promoted as better fluid choices in the resuscitation of critically ill patients. Balanced solutions have lower concentrations of chloride and use organic ions as a substitute for bicarbonate.
Studies that have compared the use of balanced solutions to 0.9% normal saline in DKA patients have demonstrated a more rapid closure of the elevated anion gap, increased mean arterial pressure, and more rapid resolution of acidemia. Depending on the specific fluid, balanced solutions also contain varying concentrations of electrolytes (i.e., potassium, calcium, magnesium).
While there are no current randomized trials that demonstrate improved mortality with the use of balanced solutions, they are a viable alternative intravenous fluid solution to 0.9% normal saline in the management of DKA.
After an initial fluid bolus, maintenance fluids should be continued at a rate of 250 to 500 mL/hour. A balanced solution should be considered for patients with hyponatremia, whereas 0.45% normal saline should be considered in patients who are hypernatremic or have normal sodium levels.
Insulin in Diabetic Ketoacidosis
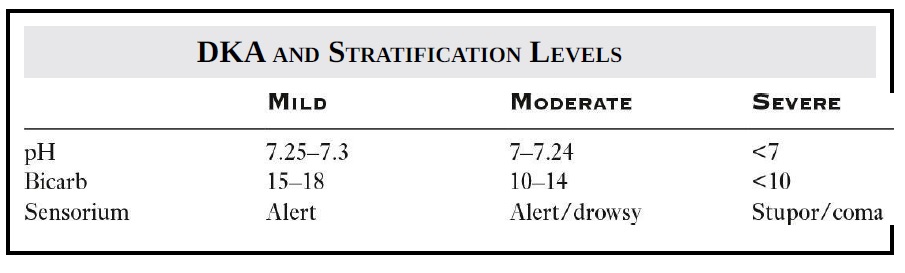
The administration of exogenous insulin is essential in the management of DKA. Insulin reverses the ketogenesis that occurs in DKA and corrects the metabolic acidosis. DKA patients can be stratified into mild, moderate, or severe based on the mental status, pH, and serum bicarbonate level. This stratification is listed in the following table :
Historically, insulin has been given as a bolus dose of 0.1 U/kg, followed by an insulin infusion. This administration strategy was felt to achieve adequate serum levels of insulin in a short period of time. Recent literature, however, has demonstrated that an initial bolus dose of insulin is not required, provided that a continuous infusion is started at a rate of at least 0.1 U/kg/h.
In addition, recent evidence has suggested that patients with mild or moderate DKA can be safely managed with intermittent subcutaneous doses of short- or medium-acting insulin preparations instead of an insulin infusion. Importantly, subcutaneous insulin administration for DKA requires further study and is not indicated in the treatment of patients with severe DKA.
Pediatric DKA patients are at risk for cerebral edema. Initiation of insulin within the first hour of treatment or prior to fluid resuscitation has been identified as a risk factor for cerebral edema. For this reason, an insulin bolus should not be administered to pediatric DKA patients. Pediatric patients should receive 1 or 2 boluses of intravenous fluids (20 mL/kg) prior to the administration of any insulin.
Insulin administration should continue until the acidosis of DKA has resolved. Once the blood glucose reaches a value of ~250 mg/dL, the type of intravenous fluid should be changed to one that contains dextrose, in order to maintain normoglycemia while the patient is treated with insulin. Once the acidosis has resolved and the anion gap is closed, a long-acting insulin should be administered via the subcutaneous route. The insulin infusion should be continued for ~1 to 2 hours after administration of the long-acting insulin in order to prevent rebound hyperglycemia or ketosis once the infusion is stopped.
Potassium in Diabetic Ketoacidosis
Many patients with DKA will have elevated levels of potassium, due to electrolyte shifts from the acidosis. However, the majority of patients are actually hypokalemic, due to loss of potassium in the urine from an osmotic diuresis. Importantly, potassium levels will decrease even further with the administration of insulin.
Potassium repletion should begin when serum potassium levels are below 5 mEq/L. If serum potassium levels are <3.5 mEq/L, potassium should be given prior to insulin administration in order to prevent life-threatening hypokalemia.
Sodium Bicarbonate in Diabetic Ketoacidosis
Contrary to conventional wisdom, the administration of sodium bicarbonate may worsen intracellular acidosis and is a risk factor for cerebral edema in pediatric DKA patients. Furthermore, bicarbonate has not been shown to improve patient-centered outcomes in the management of DKA. As a result, sodium bicarbonate is not recommended in the management of DKA, with the possible exception of cardiac arrest secondary to profound acidosis.
Read Also : Diabetic Ketoacidosis (DKA) Algorithm
Key Points
- Consider balanced fluids in the resuscitation of patients with DKA.
- An initial bolus dose of insulin is no longer recommended prior to the initiation of an insulin infusion.
- Do not administer a bolus of insulin to pediatric DKA patients.
- Do not administer insulin until the potassium level is >3.5 mEq/L.
- Sodium bicarbonate is not indicated in the treatment of patients with DKA.