Table of Contents
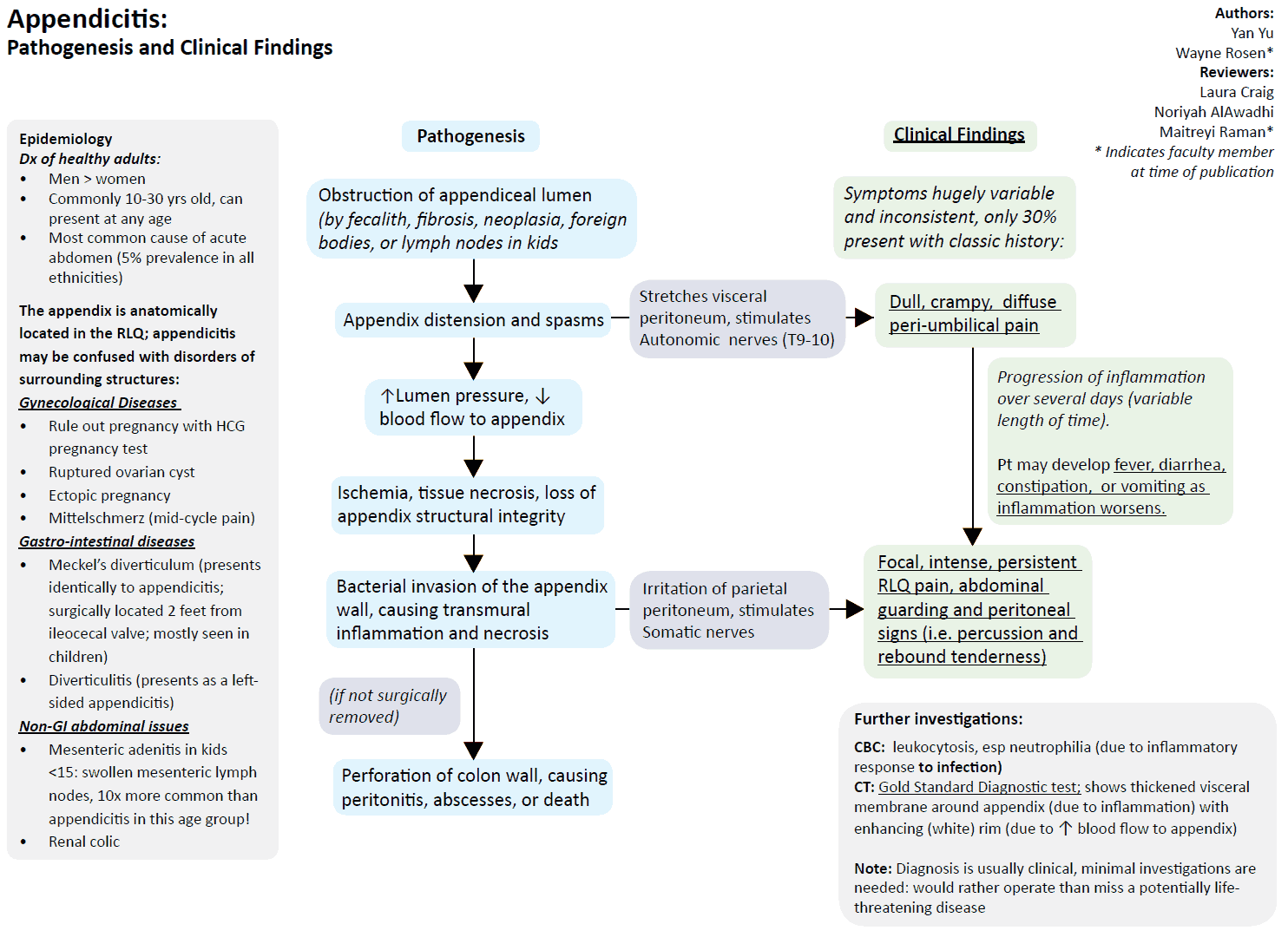
Acute appendicitis is the most common abdominal emergency. It can occur at any age, but most commonly presents during the second decade of life. Appendicitis has a male predominance, with a lifetime risk of 9% in males and 6% in females.
It occurs when there is obstruction of the appendiceal lumen, from a:
- fecalith
- tumor
- infection
- hyperplasia of lymphoid follicles
Classic symptoms of appendicitis include pain that is initially vague and periumbilical followed by a more localized parietal pain in the right lower quadrant. Only 50% of people present with these classic symptoms; in the other 50%, appendicitis can be difficult to diagnosis.
The Pain in Appendicitis
Appendicitis pain does not always occur in the right lower quadrant. Patients with congenital abnormalities may present with left-sided abdominal pain. While most patients with midgut malrotation or situs inversus totalis are diagnosed in the first month of life, some patients are not diagnosed until they present with acute appendicitis.
Retrocecal appendicitis may cause right upper quadrant pain. Retrocecal appendices are found in 26% to 65% of the population, leading to a different pattern of inflammation.
Appendiceal abscesses may develop in the pararenal space, retrocolic and paracolic gutters, and even in the subhepatic area.
Rarely, patients with acute appendicitis may present with chest pain or epigastric pain. Patients with undiagnosed congenital diaphragmatic hernia may have an inflamed appendix in the chest cavity, which would present as chest pain.
Importantly, there are three specific patient populations who are more likely to present with atypical pain from appendicitis:
- pregnant women
- children <5 years of age
- elderly patients
Acute Appendicitis in Pregnant Women
Acute appendicitis is the most common nonobstetric abdominal emergency during pregnancy. Patients may endorse burning epigastric pain, changes in bowel habits, rectal and/or vaginal pain. Nausea, vomiting, and nonspecific abdominal pain may be attributed to morning sickness in the first trimester and lead to a delayed diagnosis.
If patients are in the third trimester, the appendix is located higher up in the abdomen, and patients may complain of right flank or right upper quadrant pain.
Ultrasound (US) is 67% to 100% sensitive for appendicitis in pregnant patients if the appendix is visualized. When it is not visualized, magnetic resonance imaging (MRI) is recommended. The risk to the fetus increases if there is a delay to diagnosis and the appendix perforates (fetal loss is 20% to 30% with perforation vs. <5% without).
Acute Appendicitis in Young Children
Young children with appendicitis present differently than adults. Infants may have only lethargy and abdominal distention, while toddlers usually present with vomiting and diarrhea, which may be attributed to a viral syndrome.
Over two-thirds (70%) of children <3 years old will perforate within 48 hours due to delayed diagnosis. Moreover, two-thirds (67%) of acute appendicitis cases in young children are not diagnosed on the initial visit to a provider.
Repeat abdominal examinations will aid in diagnosis, and strong, clear return precautions for worsening pain, focal pain, or lack of resolution of symptoms are extremely important.
If there is concern for an acute appendicitis in a child or pregnant woman, US followed by MRI (if US nondiagnostic) is recommended. When the appendix is seen on MRI, there is close to a 100% sensitivity and specificity for the diagnosis of acute appendicitis. If MRI is not available, surgical consultation should nonetheless be obtained when history, examination, and laboratory studies are suspicious for acute appendicitis.
Computed tomography (CT) with its attendant risk of ionizing radiation may be an option for definitive diagnosis in both pregnancy and children, although risks and benefits should be discussed with the patient, parents, and specialty consults.
Acute Appendicitis in Elderly Patients
Appendicitis accounts for 7% of abdominal pain in elderly patients presenting to the emergency department. These patients often have multiple comorbid conditions that obscure the diagnosis.
Less than half of the patients over 60 years of age present with typical migratory abdominal pain; instead, they have vague or generalized abdominal pain. They also present to the emergency department (ED) later in the disease course, leading to higher rates of perforation.
Studies indicate that the majority of elderly patients with acute appendicitis will have already perforated by the time of surgery. This results in a very high risk of morbidity and mortality when elderly patients develop appendicitis.
CT is widely considered first line for evaluating elderly patients for appendicitis. In this population, there are a number of other potentially life-threatening diagnoses that may be detected on CT, and the long-term risks of radiation are of less concern.
Key Points
- Only 50% of appendicitis cases will present with the classic periumbilical pain migrating to the right lower quadrant.
- Patients with congenital abnormalities or retrocolic and paracolic gutters may present with right upper, left-sided, or even chest pain.
- Pregnant women, children under the age of 5, and the elderly are specific populations in whom to expect atypical presentations of appendicitis.
Suggested Readings
- Henriques de Franca Neto A, Ramos do Amorim MM, Nóbrega BM. Acute appendicitis in pregnancy: Literature review. Rev Assoc Med Bras. 2015;61(2):170–177.
- Marzuillo P, Germani C, Krauss BS, et al. Appendicitis in children less than five years old: A challenge for the general practitioner. World J Clin Pediatr. 2015;4(2):19–24.
- Omari AH, Khammash MR, Qasaimeh GR, et al. Acute appendicitis in the elderly: Risk factors for perforation. World J Emerg Surg. 2014;9:6.
- Ong EMW, Venkatesh SK. Ascending retrocecal appendicitis presenting with right upper abdominal pain: Utility of computed tomography. World J Gastroenterol. 2009;15(28): 3576–3579.
- Vissers RJ, Lennarz WB. Pitfalls in appendicitis. Emerg Med Clin North Am. 2010;28(1):103–118.