This article is an answer to the ECG Case 172
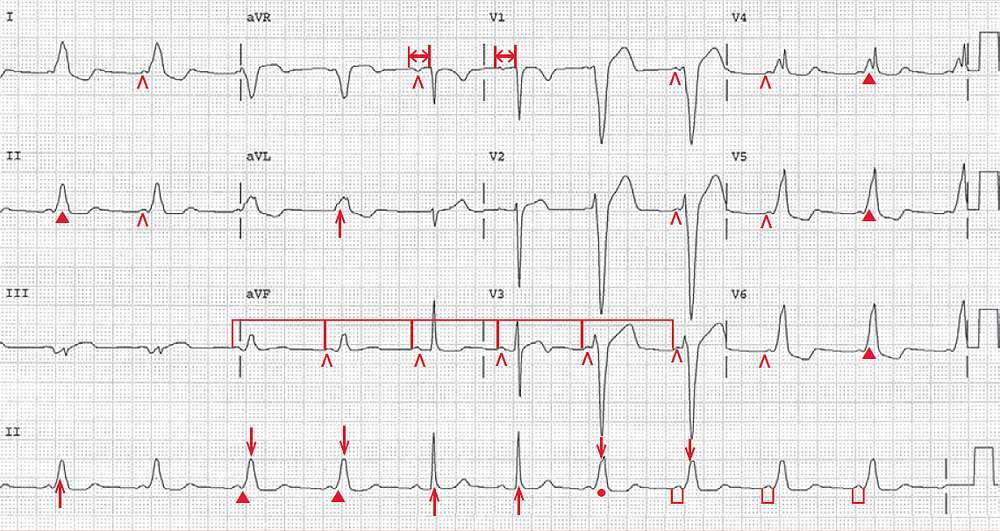
There is a regular rhythm at a rate of 64 bpm. The QRS complexes have two different durations (narrower [↑] at 0.10 sec and wider [↓] at 0.18 sec).
There is a P wave (^) before each QRS complex, and the PP intervals are constant (┌┐). The P wave is positive in leads I, II, aVF, and V4–V6. Hence there is an underlying normal sinus rhythm, but the PR intervals are not constant.
The PR interval before the narrow QRS complexes is stable (0.20 sec) (↔), while the PR interval before the wide QRS complexes are also stable, but shorter (0.10 sec) (└┘).
The narrow QRS complexes are only seen in a few leads, but they appear to have a normal morphology. The wide QRS complexes have a slurred upstroke or delta wave (▲), and along with the short PR interval, these have a Wolff-Parkinson-White (WPW) pattern. Therefore, this ECG shows intermittent WPW.
The WPW pattern represents fusion between conduction via the normal AV node–His-Purkinje system and conduction via an accessory pathway, known as a bundle of Kent, which is a connection between the atria and ventricles. The width of the QRS complex or the extent of the delta wave is determined by conduction via the AV node.
Conduction through the accessory pathway is fixed and is all or none. However, whether conduction will occur via the accessory pathway is determined by its refractoriness. If it has a short refractory period, there is likely to be conduction via the accessory pathway at all heart rates. If the refractoriness is relatively long, then conduction via this pathway may not occur when the heart rate increases.
In this situation, preexcited QRS complexes will be intermittently present. Indeed, the presence of intermittent WPW pattern, as is seen in this ECG, generally indicates that the refractoriness of the accessory pathway is relatively long, and hence rapid conduction via this pathway is not likely to occur.
In this situation, there is a decreased risk for rapid ventricular rates associated with rapid atrial rates, particularly during atrial fibrillation. It is the rapid ventricular response rate that may be 350 bpm faster and can precipitate ventricular fibrillation and hence sudden cardiac death, even in a structurally normal heart.
Also determining the presence and extent of preexcitation is conduction through the AV node. If AV nodal conduction is slow, more of the ventricular myocardium is activated via the accessory pathway and hence the delta wave is more prominent and the PR interval shorter. If AV nodal conduction is fast, then less of the ventricular myocardium is activated via the accessory pathway, and the delta wave is less prominent and the PR interval is longer.
- READ MORE: