This is an answer to the Case – Left Foot Discoloration Resolved with Elevation
A 69-year-old man presented with a 10-day history of discoloration of the left foot and pain in the left foot while at rest. He reported a 1-year history of intermittent claudication in his left leg. His medical history was notable for type 2 diabetes mellitus and hypertension.
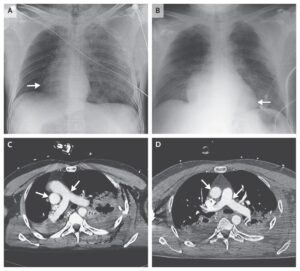
On examination, his left foot was erythematous, cold to the touch, and pulseless in the dorsalis pedis and posterior tibial arteries while hanging down. However, the foot became pale when elevated and became red again while hanging down, which is Buerger’s symptom, suggesting the presence of peripheral artery disease.
Both feet had some signs of arterial insufficiency, such as loss of hair and thin and dry skin, but there was no pallor or cyanosis.
Subsequent angiography showed severe arteriosclerosis involving the right and left external iliac arteries, with stenosis of 67% and 82%, respectively, and total thrombotic occlusion of the left superficial femoral artery.
Percutaneous transluminal angioplasty, with stent insertion in both external iliac arteries and in the left superficial femoral artery, restored the distal blood flow. After the procedure, both the redness of the left foot and the ischemic symptoms resolved.
Paradoxical redness in patients with peripheral artery disease occurs with very restricted arterial inflow and chronic dilatation of the peripheral vascular bed. The patient was well during the 3-year follow-up period, without recurrent symptoms of arterial insufficiency.