Table of Contents
Always check what the patient means by “palpitations” or clarify what you mean, as the word means different things to different people. It is usually understood as an awareness of the heartbeat.
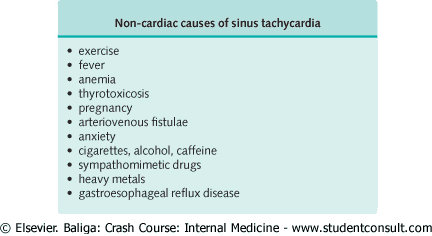
The most common cause is an arrhythmia, although other causes include conditions causing an increase in stroke volume (e.g., regurgitant valvular disease) or conditions causing an increase in cardiac output, often noncardiac causes (e.g., exercise, thyrotoxicosis, anemia, or anxiety). If an arrhythmia is suspected, try to determine whether there is an underlying cause.
Differential Diagnosis by Description of the Rhythm
Regular Rhythm
The differential diagnosis of regular palpitations includes the following:
- Heavy heart beats with normal rate: most often cardiac consciousness with sinus rhythm. It tends to be worse at rest, especially when lying in bed at night and during periods of stress.
- Fast heart rate: sinus tachycardia, atrial flutter with block, or ventricular tachycardia.
- Bursts of fast beats: paroxysmal atrial tachycardia. There is often a very long history dating back years, with a single attack followed by a long interval before the next attack. Other causes include atrial flutter, junctional rhythm, or ventricular tachycardia.
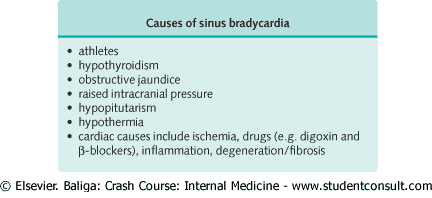
- Slow heart rate: sinus bradycardia (look for signs of hypothyroidism), atrioventricular block.
Irregular Rhythm
The differential diagnosis of irregular palpitations includes the following:
- Missed beats, “thumps”: multiple ectopics from the atrium or ventricle. The symptoms are more troublesome at rest and may disappear during exercise.
- Fast (or normal if treated): atrial flutter with variable block, atrial fibrillation (may be worse with exercise), multiple premature beats with sinus tachycardia.
History in the Patient with Palpitations
Obtain a full description of the palpitations.
- Are they continuous or intermittent?
- Are they fast, normal rate, or slow?
- Are they regular or irregular?
- When did the palpitations start?-this can vary from a few minutes to decades. Generally, if the onset dates back years and there have been no serious complications (e.g., syncope), the palpitations are usually benign.
- Often it can be helpful if the patient can tap the heart rate with a finger to represent what the patient feels.
- How often do the palpitations occur and how long do they last for? They may last for days or seconds, with intervals between episodes of a few hours to years. The patient may fear serious underlying cardiac disease, although there is usually a benign cause.
- Are there any associated features? These may be related to the underlying cause (e.g., angina, features of hyperthyroidism) or a consequence of the palpitations (e.g., faintness or dizziness).
- Always obtain a full drug history as medication is often the culprit. Ask the patient to include over-the-counter drugs and herbal supplements. This is important given the number of over-the-counter weight loss pills and other medications that contain stimulants such as caffeine or ephedra (recently banned in the U.S.).
Causal and contributory factors of Palpitations
- Ask about smoking, alcohol, and caffeine (tea, coffee, cola) intake. These may contribute to extrasystoles.
- Myocardial ischemia may lead to any supraventricular or ventricular arrhythmia.
- Digoxin, which is commonly used to control atrial fibrillation, may also cause any arrhythmia, especially in the presence of hypokalemia. Note that most antiarrhythmic agents also have a proarrhythmic effect.
- Ask about rheumatic heart disease as atrial fibrillation often accompanies mitral stenosis.
Noncardiac causes of palpitations include the following:
- Thyrotoxicosis: may cause sinus tachycardia, paroxysmal atrial tachycardia, atrial flutter/fibrillation. Ask about hyperthyroid symptoms such as sweating, tachycardia, weight loss, and tremor.
- Anemia: ask about anticoagulant usage, recent history of hematemesis, melena, heavy menorrhea.
- Myxedema: may be responsible for sinus bradycardia.
- Anxiety: a very common cause of palpitations.
Consequences of Palpitations
Palpitations may not affect the patient or may just be a minor nuisance. If a benign arrhythmia is present, reassurance that the condition is not serious is often all that is required.
Changes in rate may be more serious, compromising coronary blood supply and leading to symptoms of myocardial ischemia or cardiac failure.
Tachycardia or bradycardia may lead to a reduction in cardiac output and cause dizziness or collapse (e.g., Stokes-Adams attacks in complete heart block).
Prolonged tachycardia may also lead to Tachycardia-induced cardiomyopathy (TIC).
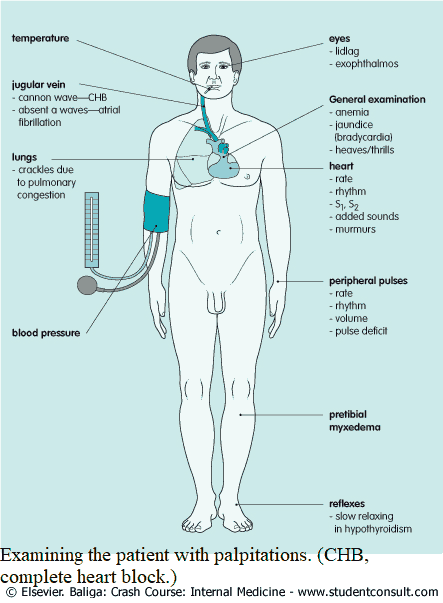
Examining the Patient with Palpitations
- Look for signs of anemia and hypo/hyperthyroidism (tremor, nervousness).
- Examine the limbs for signs of DVT, since PE can cause arrhythmias.
- Feel the pulse. Note the following:
- Rate: beats per minute. Rhythm: regular, regularly irregular (e.g., Wenckebach second-degree heart block),
- Irregularly irregular (e.g. multiple ectopic beats or atrial fibrillation).
- Volume (e.g., a collapsing pulse of hyperdynamic circulation or a slow volume pulse of shock or aortic stenosis).
- If the patient is symptom free at the time of examination, the pulse may be normal.
- The blood pressure will be low if the arrhythmia leads to a reduction in cardiac output. Hypertension may predispose to atrial fibrillation.
- The jugulovenous pressure may be elevated if cardiac failure is present. Cannon A waves are visible with complete heart block, and A waves are absent in atrial fibrillation.
- Feel for heaves and thrills with associated right ventricular enlargement and valvular heart disease.
- Assess the rate and rhythm by auscultation. The peripheral pulse rate may be slower than the apical rate in atrial fibrillation (pulse deficit). The first heart sound is of variable intensity in heart block and atrial fibrillation. Listen for cardiac murmurs, e.g., evidence of mitral valve disease predisposing to atrial fibrillation. Focus on any abnormal findings
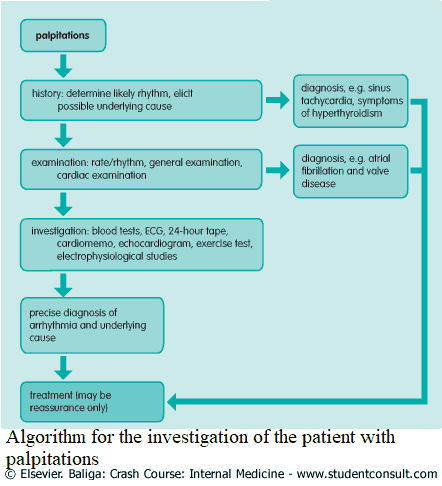
Investigating the Patient with Palpitations
Blood Tests
- Complete blood count: anemia.
- Metabolic panel: especially disturbances of potassium; less commonly, magnesium deficiency may contribute to refractory arrhythmias.
- D-dimer: to rule out PE.
- Thyroid function tests: hypo/hyperthyroidism.
- Drug concentration if appropriate (e.g., digoxin levels).
Other Tests
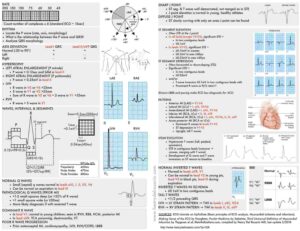
- Electrocardiogram (ECG): mandatory for anyone with palpitations and can often reveal the precise nature of the palpitations if present.
- 24-hour ECG: for intermittent symptoms. It should be carried out with a diary of symptoms to see if they correlate with any rhythm disturbances found.
- Palpitations memo: if symptoms do not occur every day, a palpitations memo can record the heart rhythm by phone at the press of a button.
- Echocardiogram: to exclude any underlying valvular disease.
- Holter monitor: if symptoms do not occur every day, a Holter monitor or event monitor can record the heart rhythm by phone at the press of a button or for a set duration of time.
- Chest x-ray: can show cardiomegaly, suggesting heart failure; also shows pulmonary causes.
- Stress test: the induction of symptoms, under controlled conditions with ECG monitoring, may be appropriate.
- Electrophysiologic studies: more rarely, patients may be referred for specialized studies. These can be used to induce arrhythmias, locate the origin of the arrhythmic focus, and to assess the response to drug treatment.