Table of Contents
General and Airway
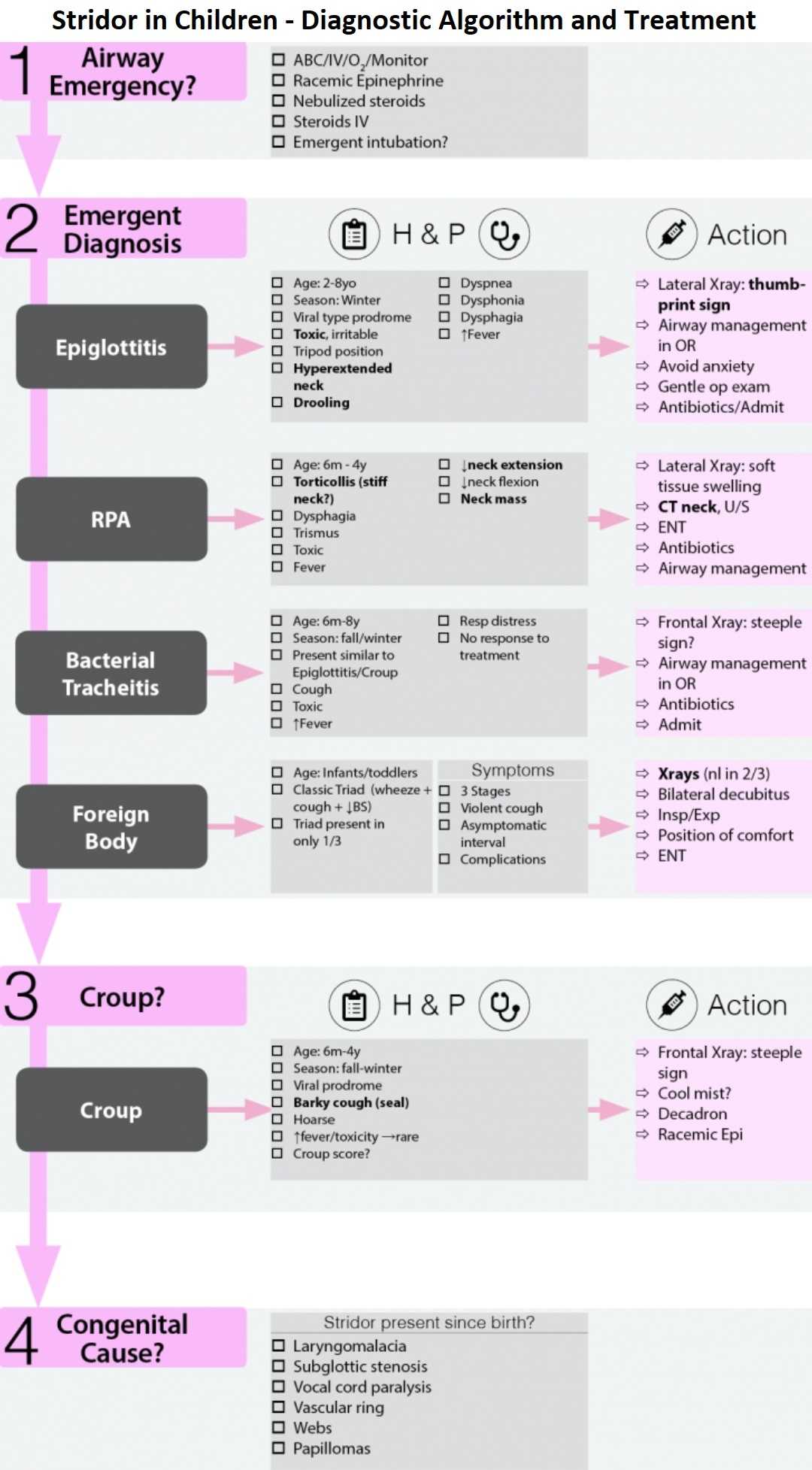
Empiric treatment of Stridor in Children
- Racemic Epi
- Nebulized steroids
- Steroids IV
- Emergent intubation?
Types of stridor:
- Inspiratory → subglottic
- Expiratory → supraglottic
- Biphasic → subglottic, glottic
- Sonorous → nasal
Rule Out Emergent Diagnosis and Causes of Stridor in Children
- Epiglottitis
- Retropharyngeal Abcsess
- Bacterial Tracheitis
- Foreign Body Aspiration
1. Epiglottitis
Definition of Epiglottitis
- Acute inflammation of epiglottis and surrounding structure → serious, life threatening, airway emergency
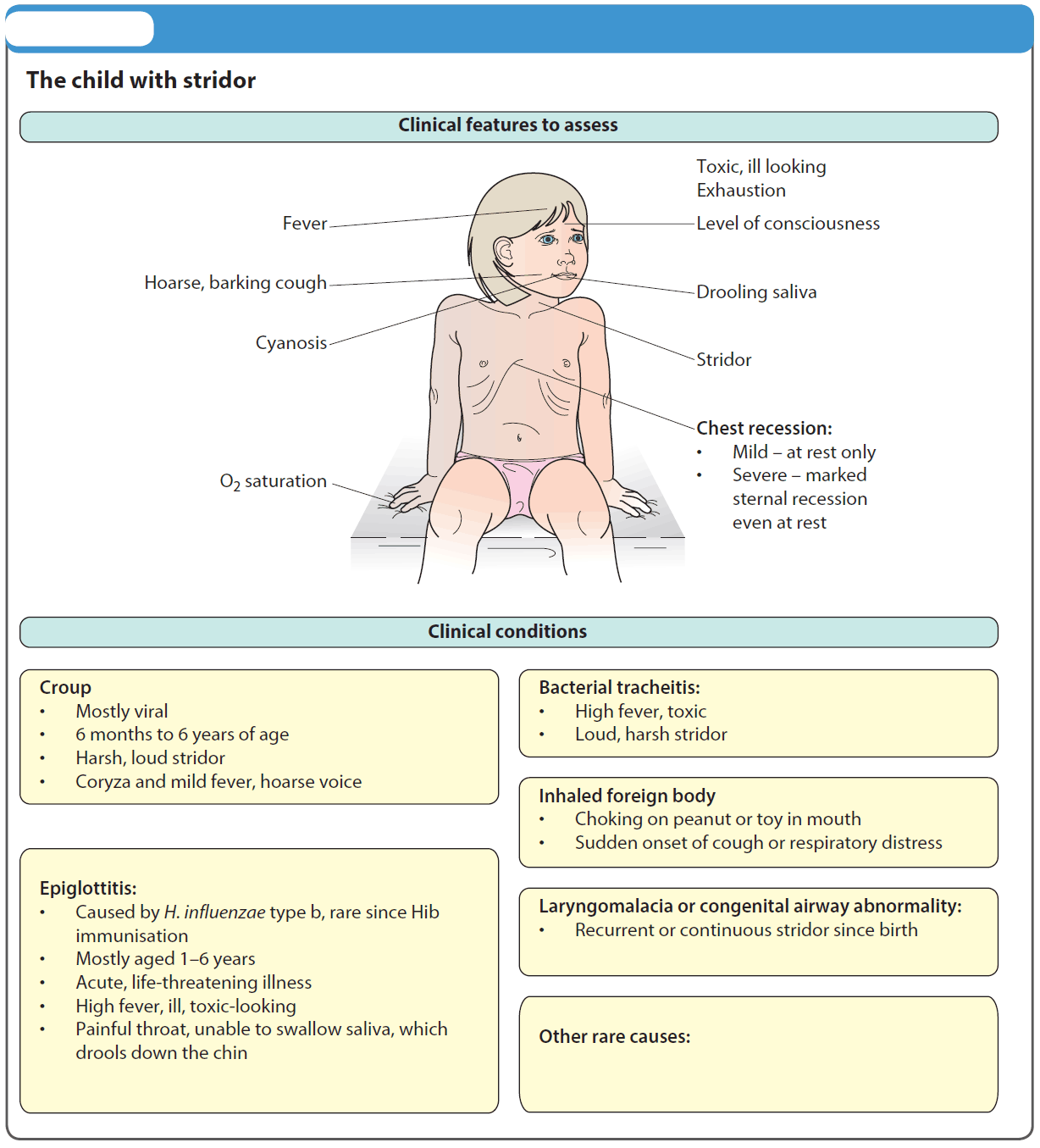
Clinical
- Age: 2-8yo; Season: Winter
- Viral type prodrome
- Toxic, irritable, fever
- Tripod position, hyperextended neck
- The D’s: Drooling, Dyspnea, Dysphonia, Dysphagia
Diagnosis of Epiglottitis
- Lateral neck Xray → “thumb print sign”
- Can be negative in up to 20% of cases (Prim care 1990;17(2):335-45)
- Diagnosis made on visualization of inflamed epiglottis
Treatment of Epiglottitis
- Avoid agitation of child as this can worsen the airway (no IV, oral examination)
- If emergent airway needed → use tube size 0.5-1 smaller than age
- Ideal airway should be obtained in the OR, controlled conditions
- Antibiotics (3rd gen Cephalosporin)
2. Retropharyngeal Abcsess
General
- Clinical Presentation similar to meningitis but usually has normal mental status
- Pathology: Deep neck space infection (URI vs penetrating trauma to oropharynx), can spread through neck → danger space → cause mediastinitis
Clinical
- Torticollis (stiff neck?) (36.5%)
- ↓ Neck extension (45%), ↓ Neck flexion (12.5%)
- Dysphagia
- Trismus, toxic, fever
- Stridor rare (3%)
- Age:
- 50% of cases occur between 6-12mos, 96% occur before 6 years of age (Arch Dis Child 1991;66:1227-30)
- Lymph nodes of Rouviere that drain the retropharyngeal space atrophy after 6 years
- Appearance: Child with neck in neutral, difficulty extending neck and uses eyes to look up
- Often confused with meningitis:
- ↓ Neck flexion in meningitis vs. ↓neck extension in RPA (Pediatrics 2003;111:1394-8)
Fever, Stiff Neck, Altered Menal Status ?
Consider Retropharyngeal Abcsess along with meningitis!!! (Similar presentations)
Work-up for Retropharyngeal Abcsess
- Xray, lateral neck
- Low yield, not widely used
- CT neck
- Helps localize where problem is
- Difficult to differentiate between pus and cellulitis
- US neck
- May help distinguish between purulence vs adenitis vs abscess
Treatment of Retropharyngeal Abcsess
- ENT Consultation
- Antibiotics (alone treat 37%):
- Clindamycin
- OR if not improve
Complications of Retropharyngeal Abcsess
- Airway compromise
- Descending necrotizing mediastinitis
- Spread from Retropharyngeal space → retrovisceral space → pierce alar fascia → Danger space
- Rare in children
- Internal jugular vein thrombosis
- Mycotic aneurysms
3. Bacterial Tracheitis
General
- Croup-like illness + toxic + not respond to therapy
- Pathology: laryngeotracheobronchitis, subglottic edema and membranous secretions
Clinical
- Bacterial Tracheitis vs epiglottitis (J Otolaryngol 1989;18(3):101-4)
- Tracheitis children have a cough, comfortable lying down, no drool
- Age: 6m-8y; Season: fall/winter
- Present similar to Epiglottitis/Croup
- Cough, toxic, fever, respiratory distress
- No response to treatment
Diagnosis of Bacterial Tracheitis
- Frontal neck X-ray → Steeple sign (non-specific finding)
- Endoscopic visualization of normal supraglottic structures and subglottic inflammation, pus in airway, ulcers, secretions
Treatment of Bacterial Tracheitis
- Emergent airway → use tube size smaller than what is appropriate for their age
- Ideally intubated , diagnosed, cultured in the OR under optimal conditions
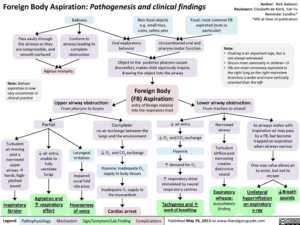
4. Foreign Body Aspiration
Clinical
- Age: Infants/toddlers
- Classic Triad (wheeze + cough + decreased breath sounds) present in only 1/3
- Symptoms (3 stages)
- Violent cough
- Asymptomatic interval
- Complications
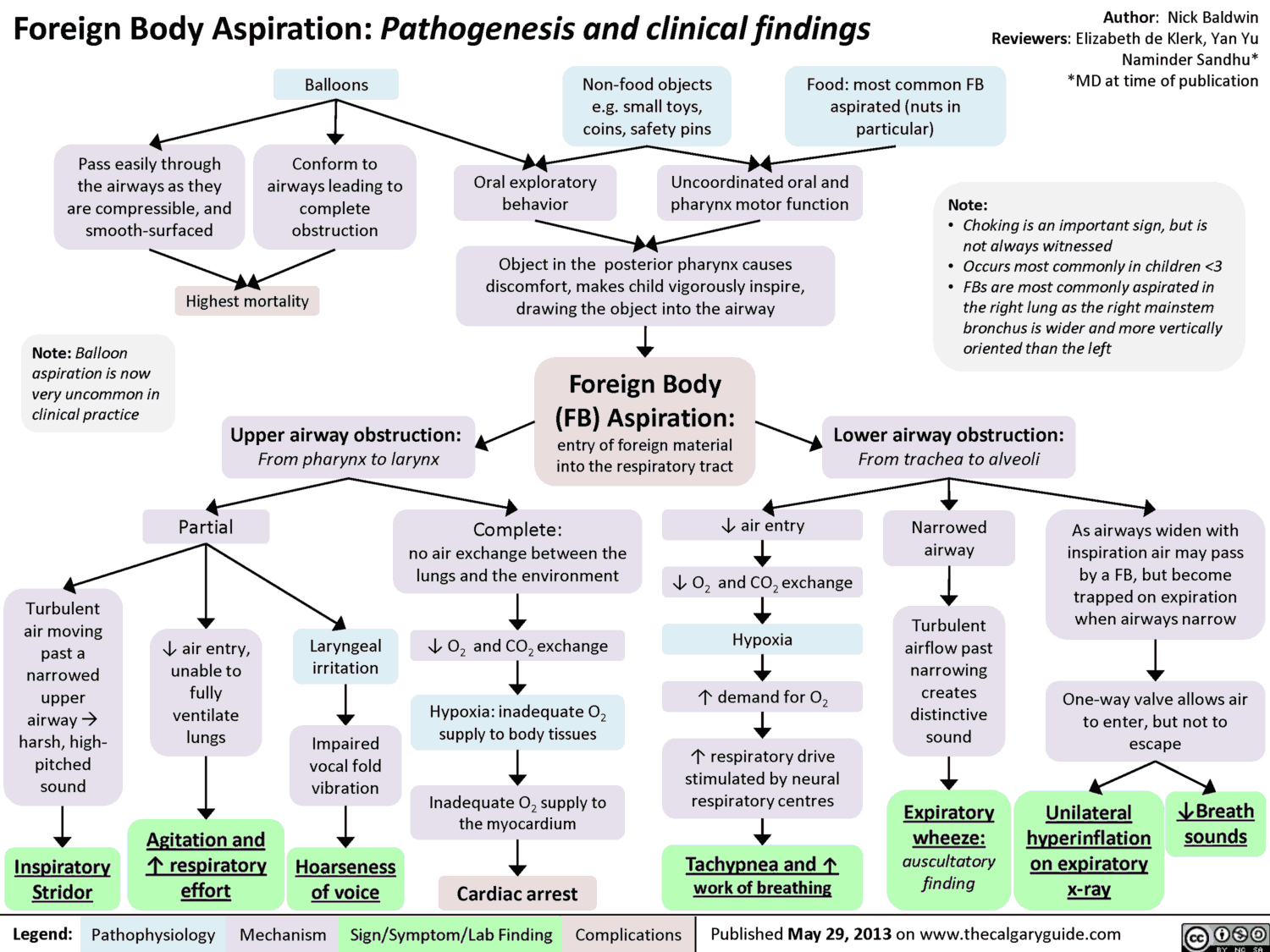
Diagnosis of Foreign Body Aspiration
- History
- Only 50% diagnosed in first 24h
- Usually asymptomatic in ED
- Witnessed foreign body aspiration?
- Elicit a choking/coughing episode in the history (sudden onset dyspnea/choking/cyanosis)
- Xrays (normal in 2/3)
- Sensitiivty 68%, specificity 68% (Pediatr Radiol 1989;19:520)
- Bilateral decubitus (not helpful)
- Insp/Exp
- CT
Treatment of Foreign Body Aspiration
- Position of comfort
- ENT
- Referral for bronchoscopy
Complications of Foreign Body Aspiration
- Obstruction, infection, fever, cough
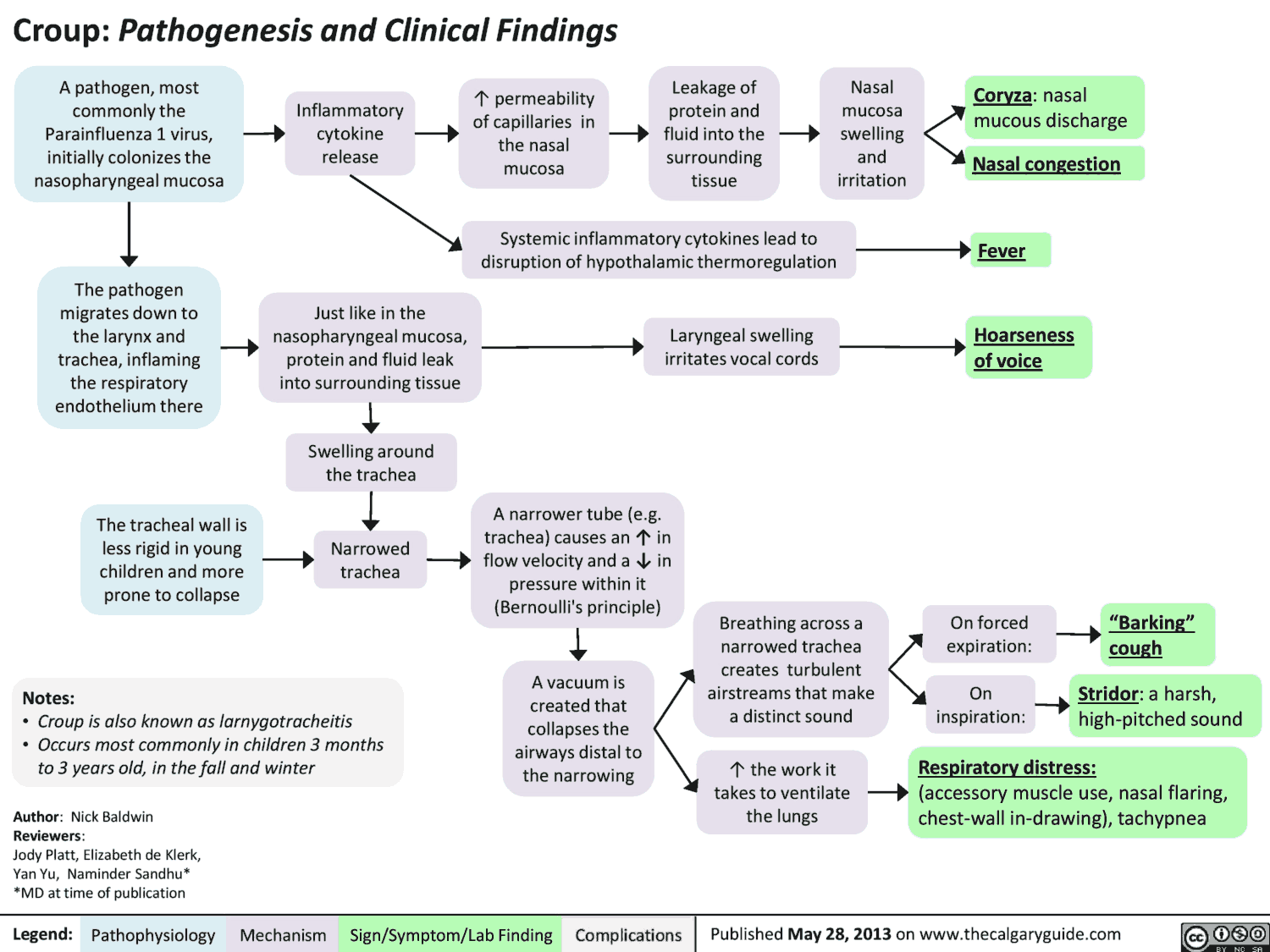
Croup
General
- Peak incidence in 1-2 year
- Organisms: Parainfluenza I (most common-80%), II and III, M. pneumoniae, RSV, Influenza (severe form), adenovirus
Clinical features of Croup
- Age: 6m-4y; Season: fall-winter
- Viral prodrome
- Barky cough, hoarse (subglottic airway narrowing)
- Fever: common in croup, but usually not toxic
- Lateral Neck Xray: Steeple sign (non-specific finding)
- Croup score? (See table)
- Symptoms peak over 2 days and resolve over 1 week
- Croup score: mild (0-4), mild/mod (5-6), moderate (7-8), severe (9-14), terminal (15)
| Croup Score | 0 | 1 | 2 | 3 |
| Color | Normal | Dusky | Cyanotic | Cyanotic on O2 |
| Air movement | Normal | Mild | Moderate | Marked |
| Retractions | None | Mild | Moderate | Severe |
| Mentation | Normal | Restless | Lethargic | Obtunded |
| Stridor | None | Mild | Moderate | Severe |
Treatment of Croup
- Cool mist
- Sooths inflamed mucosa
- Multiple studies show minimal efficacy in treating croup (JAMA 2006;295(11):274)
- Generally not helpful
- Steroids
- Indication: all croup in the ED?
- Decreased mortality for croup from 1/200 to 1/30,000
- Multiple studies show efficacy, associated with a decrease in ED stay and ED bounce backs (Ann Emerg Med 2002;30(3):353)
- Efficacious for even mild croup, less likely to return for croup related care (NEJM 2004;351(13):1306)
- Dose:
- 0.15mg/kg vs 0.3mg/kg vs 0.6mg/kg?? (Max 10 mg)
- All equally efficacious PO or IM or inhaled (Acad Emerg Med 2003;10:16)
- IV formulation can be given po
- Racemic epinephrine
- Indication: mod/severe croup; stridor at rest → can help reduce need for emergent intubation
- Dose: 0.25-0.5ml of 2.25% solution with saline to total of 3ml
- Racemic Epineprine vs Epinephrine?
- Equivalent: substitute with epinephrine 0.5ml /kg of 1:1000, 5ml max with equal efficacy (Pediatrics 1992;89(2):302) (Cochrane Database Syst Rev. 2011 Feb 16)
- Rebound phenomenon?
- No need for admission for observation, if significantly improved → can be safely discharged after 3 hours (Ann Emerg Med 1995;25:331-7)
- Repeat Epinephrine
- Usually 2 doses of epinephrine = Admit
- But, if they respond to the 2nd epinephrine, well-appearing and observed 2-4 hours without decompensation → can possibly discharge home
- Summary: may give cool mist, steroids for all kids in ED, epinephrine only if they have stridor.
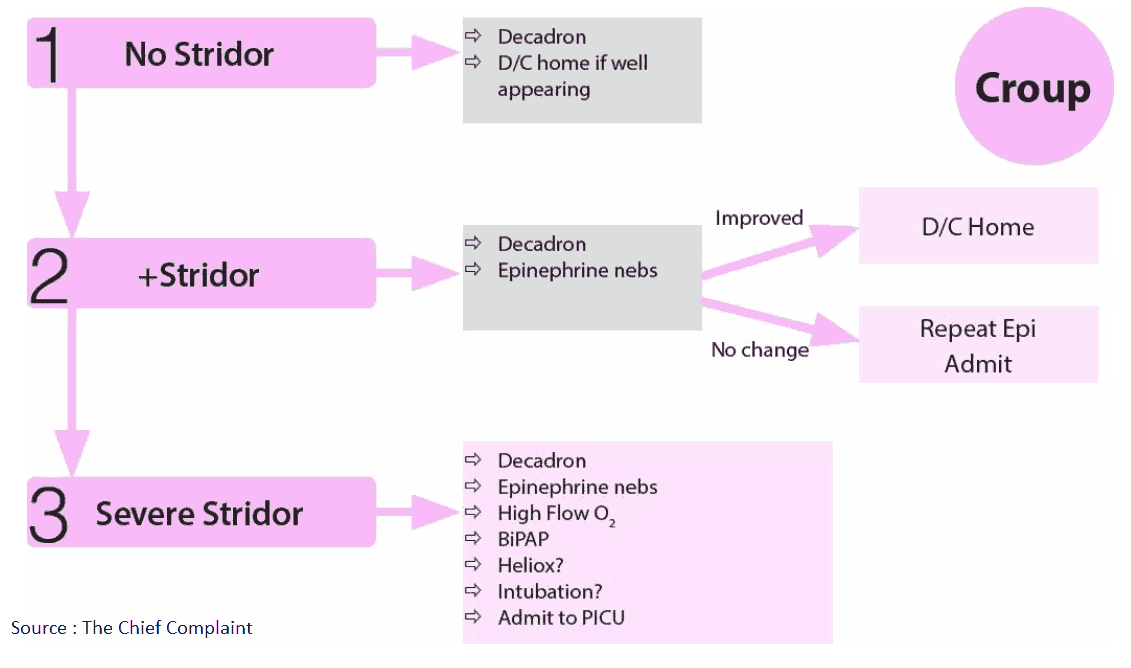
Disposition
- Discharge: well-appearing, normal color, no stridor at rest, no ALOC (Altered Level of Consciousness)
- Admit: Moderate croup score, toxic appearing, respiratory distress, received more than 2 doses of nebulized epinephrine
Discharge Criteria:
– Good PO intake
– RR < 40
– Sat > 94%
– Well appearing
Consider Congenital Causes of Stridor in Children
Stridor present since birth? Congenital Causes of Stridor:
- Laryngomalacia
- Subglottic stenosis
- Vocal cord paralysis
- Vascular ring
- Webs
- Papillomas
References
- Pharyngitis, croup, and epiglottitis. https://pubmed.ncbi.nlm.nih.gov/2196614/
- Retropharyngeal Abscess in Children: Clinical Presentation, Utility of Imaging, and Current Management. https://pediatrics.aappublications.org/content/111/6/1394.short
- Retropharyngeal abscess. https://adc.bmj.com/content/66/10/1227.abstract
- Bacterial tracheitis in children. https://pubmed.ncbi.nlm.nih.gov/2654411/
- How accurate is chest radiography in the diagnosis of tracheobronchial foreign bodies in children? https://link.springer.com/article/10.1007/BF02389562
- A Randomized Trial of a Single Dose of Oral Dexamethasone for Mild Croup. https://www.nejm.org/doi/full/10.1056/nejmoa033534
- Intramuscular versus Oral Dexamethasone for the Treatment of Moderate-to-severe Croup: A Randomized, Double-blind Trial. https://onlinelibrary.wiley.com/doi/abs/10.1197/aemj.10.1.16
- Prospective randomized double-blind study comparing L-epinephrine and racemic epinephrine aerosols in the treatment of laryngotracheitis (croup). https://pubmed.ncbi.nlm.nih.gov/1734400/
- Safety and efficacy of nebulized racemic epinephrine in conjunction with oral dexamethasone and mist in the outpatient treatment of croup. https://pubmed.ncbi.nlm.nih.gov/7864472/