Table of Contents
General Approach
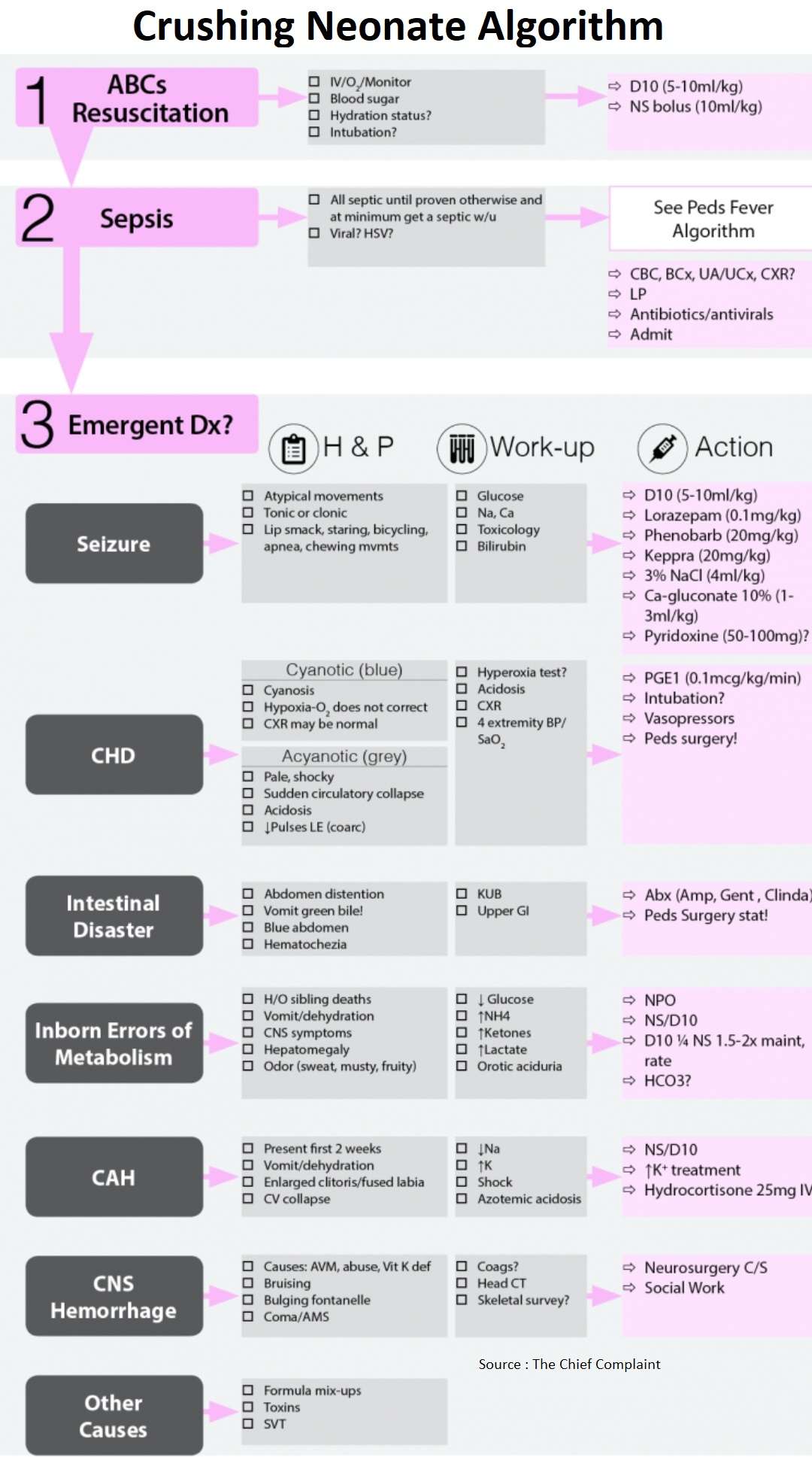
- Definition: Full-term newborn, born well and discharged home by pediatrician → returns in first month looking sick, hypotensive and dehydrated.
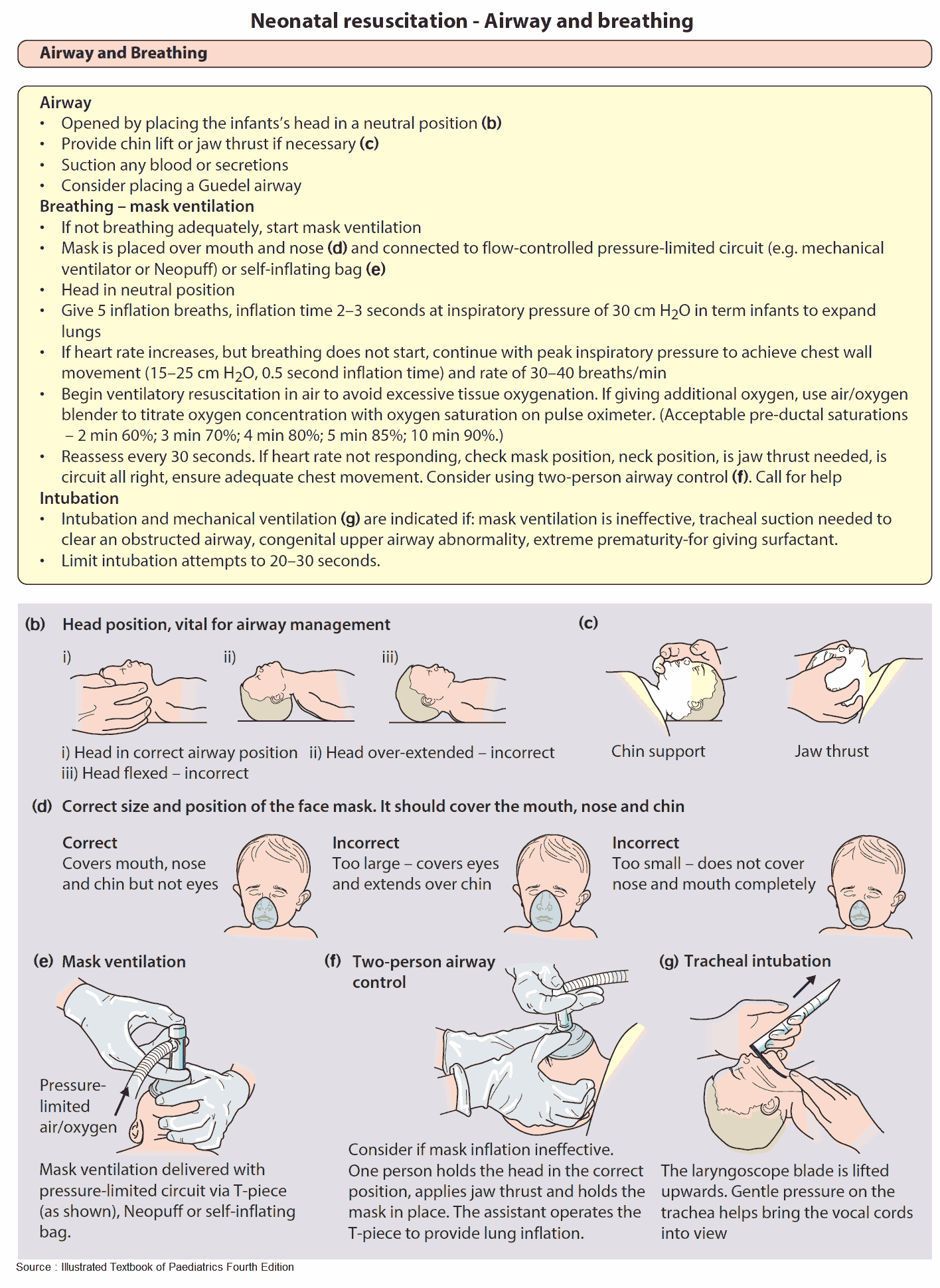
- Always begin with ABCs and decide whether or not to emergently intubate.
- Begin fluid resuscitation if not in overt CHF and check/correct hypoglycemia.
- Consider and rule-out emergent causes starting with focused H&P, labs and possibly imaging.
- At minimum, these neonates will get a septic work-up including labs, antibiotics and possibly LP, then admission.
ABCs and Resuscitation
Resuscitation
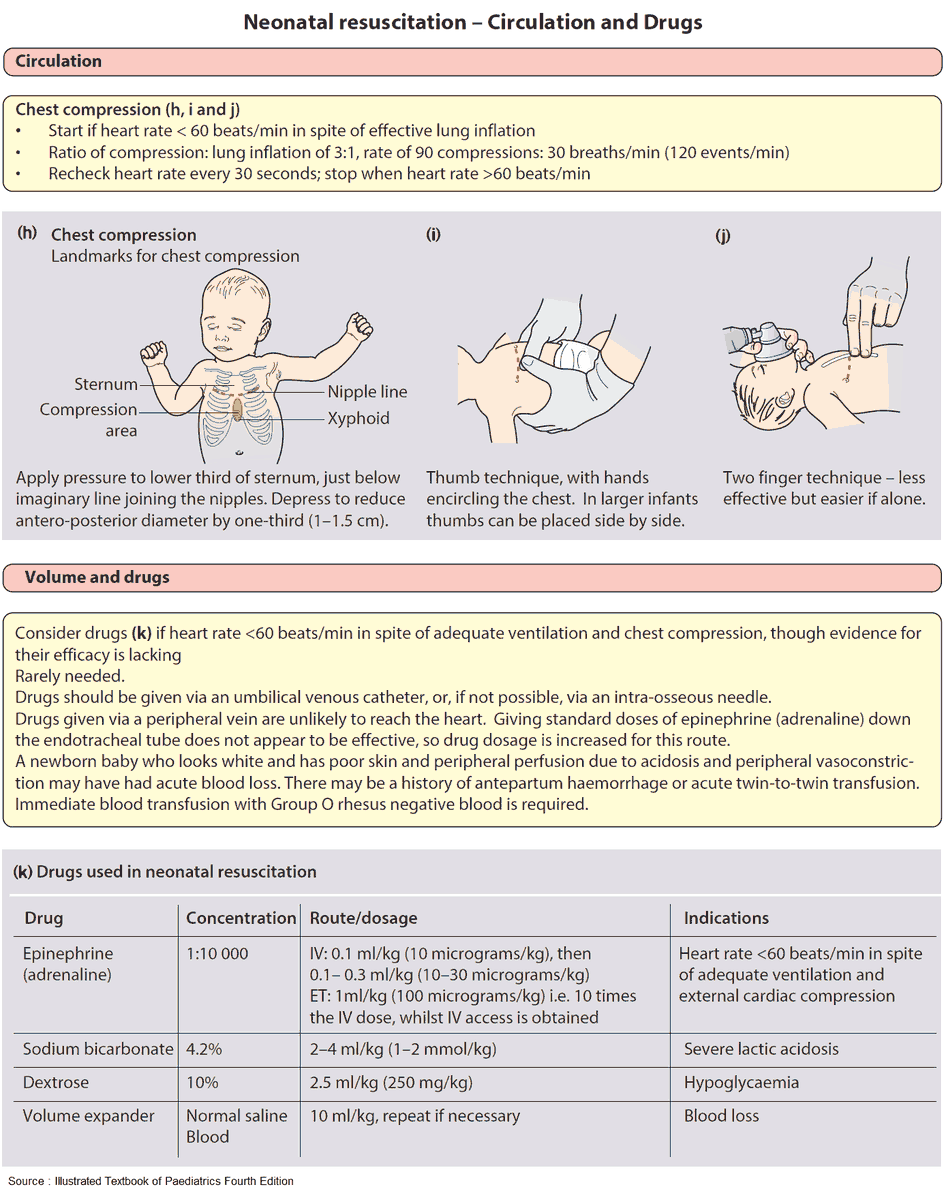
- Early IV access
- Scalp vein, IO line, umbilical line
- Vital signs:
- 4 extremity Blood Pressure; Pre and post ductal O2 saturation
- Minimally acceptable SBP = 60 mmHg
- Initial labs
- Full sepsis work-up (Accucheck, CBC/CMP/BCx/Lactate/NH4/UA/UCx)
Treat reversible causes
- Hypoglycemia always present → treat early with D10 (5-10ml/kg IV)
- Begin fluid resuscitation → NS boluses (10ml/kg IV)
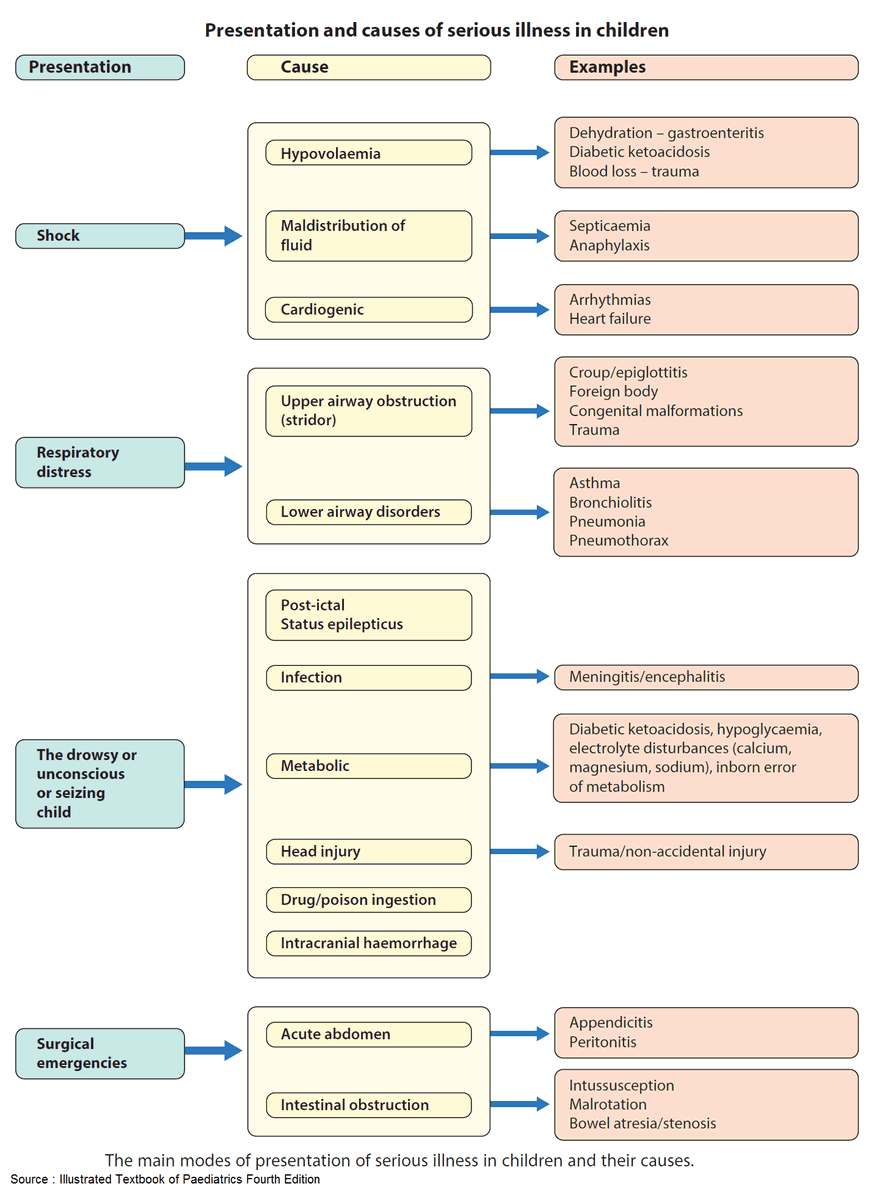
Differential Diagnosis : THE MISFITS
– Trauma
– Heart disease/Hypovolemia
– Endocrine (CAH)
– Metabolic (electrolytes)
– Inborn errors metabolism
– Seizures
– Formula mishaps
– Intestinal disaster
– Toxins
– Sepsis
Begin Neonatal Sepsis Work-up
Full septic work-up
- All ill appearing neonates are septic until proven otherwise
- CBC, LFTs, BCx
- Urine Analysis/Urine culture
- CSF studies-LP
- CXR
- Antibiotics
- Cefotaxime 50-100mg/kg
- Ampicillin 75mg/kg
- Vancomycin 15mg/kg
- +/- Acyclovir 20mg/kg
- Admit
Emergent Differentials
- Seizures
- Congenital Heart Disease
- Intestinal Emergencies
- Inborn Errors of Metabolism
- CAH (Congenital Adrenal Hyperplasia)
- Non-Accidental Trauma
1. Seizures
Presentation of Seizures in Neonate
- Atypical seizure
- Presents with atypical movements → usually not tonic-clonic
- Usually staring spell, lip smacking, bicycling, tonic, migratory clonic
Diagnosis of Seizures in Neonate
- Differential diagnosis is large: (Emerg Med Clinics North Am 2002;20:27-48)
- Hypoxic-Ischemic encephalopathy → most common cause(50-65%)
- Intracranial hemorrhage: IVH/SDH/SAH (15%)
- Electrolyte abnormalities: Hypercalcemia, Hyper and Hyponatremia, Hyperphophatemia, Hyper and Hypoglycemia
- Other: Infection, IEM, metabolic, drug withdrawal, toxins, trauma, hypertension, formula mix-up (Hyponatremia)
- Work-up
- Labs
- Check labs even if seizures have stopped
- Check glucose immediately
- Check and correct Natriuum, glucose, Calcium
- CT Head
- Sepsis work-up
- Labs
Treatment of Seizures in Neonate
- Correct hypoglycemia: D10: (5 to 10 ml/kg)
- Benzodiazepines: Lorazepam 0.1mg/kg initial drug of choice
- Anticonvulsant
- Phenobarbital 20mg/kg IV
- Levetiracetam (Keppra) 20mg/kg IV
- Fosphenytoin 15-20 mg/kg IV
- Treat hypocalcemia (≤7mg/dl): Ca gluconate 10% (100–300 mg/kg IV)
- Treat hyponatremia (<125 mg/dl): 3% saline (4 ml/kg)
- Pyridoxine (50-100mg)
- Consider if refractory seizures
- Sepsis
- Begin sepsis work-up and broad antibiotics (see peds fever algorithm)
- Treat for HSV (Lumbar Puncture and begin acyclovir)
2. Congenital Heart Disease (CHD)
General
- Neonate with congenital heart disease may rely on a patent ductus arterious (PDA) to shunt blood for pulmonary blood flow or systemic blood flow
- PDA usually closes within 2 weeks → ductus arteriosus no longer able to shunt blood past
- CHD lesion → rapid clinical deterioration depending on site of lesion
- May have ductal dependent pulmonary blood flow (Cyanotic CHD) or ductal dependent systemic blood flow (Acyanotic CHD)
Cyanotic CHD (Congenital Heart Disease)
- General
- Ductal dependent pulmonary blood flow
- When duct closes → low pulmonary blood flow → low O2 to body → infant becomes cyanotic/blue
- Cardiovascular consult immediately → OR?
- Diagnosisof Cyanotic CHD
- Physical Exam: Cyanosis (blue baby)
- Hypoxia
- Low O2 saturation → likely ductal dependent lesion
- Hyperoxia test:
- i. 10-15 min of 100% FiO2
- ii. If ABG PaO2 <150 → indicative of cyanotic CHD
- CXR
- Rule out other causes for hypoxia
- Treatmentof Cyanotic CHD
- O2
- PGE1
- IV fluids if hypotensive
- Vasopressors: Dopamine/Dobutamine if needed
Acyanotic CHD
- General
- Ductal dependent systemic blood flow
- When duct closes → low blood flow to body → shock
- Likely lesion: critical coarctation, aortic stenosis, hypoplastic LV
- DiagnosisofAcyanotic CHD
- Shock?
- Poor perfusion, tachycardia, hypotension
- 4 extremity Blood Pressure and SaO2
- Look for gradient between extremities
- Shock?
- TreatmentofAcyanotic CHD
- PGE1
- IV Fluids if not in CHF
- Vasopressors: Dopamine, Dobutamine, Milrinone
Treatments of Congenital Heart Disease (CHD)
- PGE1
- Dose: 0.1 mcg/kg/min
- Side effects
- Hypotension
- Apnea
- i. Dose-dependent and occurs early
- ii. May need to intubate before transfer (do not stop PGE1)
- Check for clinical improvement → Perfusion, pH, BP, SaO2, Urine output
- Vasopressors
- Cyanotic CHD:
- Dopamine/Dobutamine
- Acyanotic CHD:
- Dopamine/Dobutamine (5-10 mcg/kg/min), Milrinone
- Do not use Levophed or Epinephrine → may worsen coarctation
- Cyanotic CHD:
- Other
- IV fluids
- Acidosis? → Consider HCO3 for pH < 7.0
- Anemia? → Consider transfusion
3. Intestinal Emergencies
VOLVULUS IN NEONATE
- PresentationofVolvulus
- Congenital malrotation
- Irritable, vomiting: gastroenteritis symptoms
- Unexplained Bilious Vomiting in young infant = malrotation and midgut volvulus until proven otherwise
- Work-upfor Volvulus
- Urinary X-Ray: usually normal but can have ”double-bubble” sign with severe duodenal obstruction
- Upper gastrointestinal X-Ray : corkscrewing of intestine
- TreatmentofVolvulus
- Antibiotics
- Surgical emergency!
- Complete volvulus can lead to bowel necrosis in 1-2 hours! (Emerg Med Clinics North Am 2002;20:139-153)
Vomit Pearl
Bilious vomit = Volvulus
NECROTIZING ENTEROCOLITIS
- Usually in premature but can be in full term infants
- Presentation: similar to volvulus → feeding difficulties, irritability, abdominal distention, and hematochezia
- X-Ray
- Low sensitivity – usually normal
- Late: pneumatosis intestinalis (gas in bowel wall) or portal free air
- Therapy: Bowel rest, antibiotics, surgical consultation
Other Intestinal emergencies in Neonate
- Incarcerated hernia
- Diaphragmatic hernia
- Toxic Megacolon
- Duodenal atresia
- Pyloric stenosis
Treatment for all
- ABCs and resuscitation: Saline and Dextrose as above
- NPO
- Antibiotics
- Upper GI contrast study
- Surgical Consult
4. Inborn Errors of Metabolism
Pathophysiology of Inborn Errors of Metabolism
- Biochemical defect that causes accumulation of toxic metabolite (NH4, ketones, lactic acid)
Presentation of Inborn Errors of Metabolism
- Aleterd Mental Status, vomiting, lethargy, coma, dehydration
- History of sibling deaths
- CNS symptoms
- Hepatomegaly
- Odor (sweat, musty, fruity, like urine)
- Family history of siblings with same presentation?
Work-up and treatment of Inborn Errors of Metabolism
- Labs
- Hypoglycemia
- ↑ NH4 (Hyperammonemia)
- Ketonemia (Ketosis)
- High Lactate
- NPO
- Hypoglycemia: D10 (5-10ml/kg IV)
- Rehydrate
- Bolus: 10cc/kg NS boluses
- Maintenance: D10 ¼ NS 1.5-2x maint rate after fluid boluses
- HCO3 ? (if pH<7.1 for organic acidemia)
5. CAH (Congenital Adrenal Hyperplasia)
Pathophysiology of CAH
- 21-hydroxylase deficiency (90%)
- Deficiency in cortisol and aldosterone → hyponatremia, hyperkalemia
- Accumulation of androgens → changes in female genitalia
Presentation of CAH
- Vomiting, dehydration, lethargy, decreased po intake
- Shock in the first 2 weeks of life
- Hyponatremia, hyperkalemia and hypoglycemia
Treatment of CAH
- Hypoglycemia treatment → D10 (5 to 10 ml/kg)
- Resuscitate: 10cc/kg NS boluses
- Treat hyperkalemia
- Ca-gluconate for hyperK and EKG changes
- Steroids: Hydrocortisone 25mg IV/IM/IO
6. Non-Accidental Trauma
- Presentation
- May have no external signs of trauma
- Scalp hematoma → associated with high risk of intracranial hemorrhage
- Retinal hemorrhages
- Work-up
- CT head
- Admit
- Social work/child services
Other Causes of Crashing Neonate
- NAT (Non accidental Trauma)
- Arrhythmias
- Formula-mix ups
- Omphalitis
- AVM (Arteriovenous Malformation)
- Bronchiolitis
References
- Common complaints in the first 30 days of life. https://www.emed.theclinics.com/article/S0733-8627(03)00050-6/fulltext
- Common abdominal emergencies in children. https://pubmed.ncbi.nlm.nih.gov/11826631/