This article is an answer to the ECG Case 162
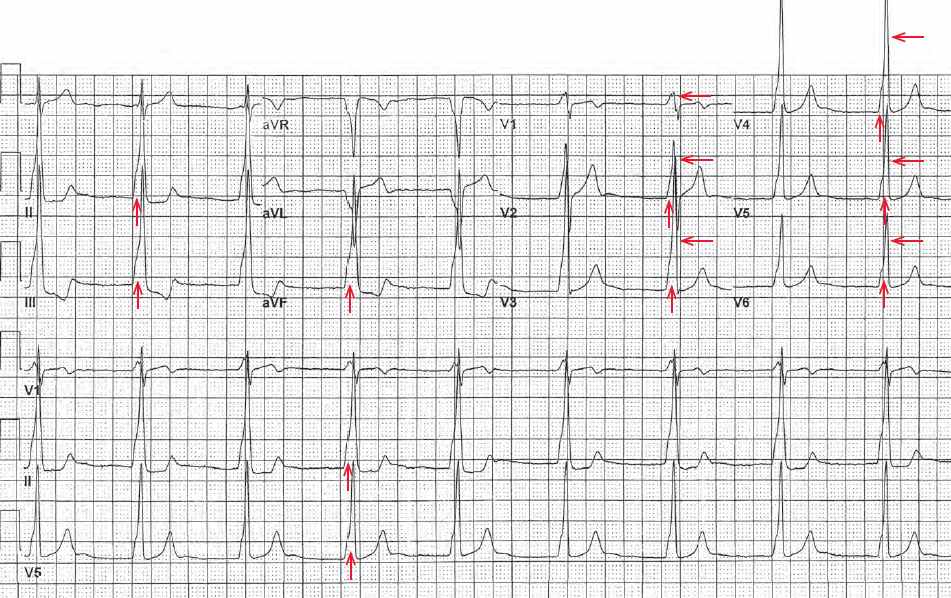
The ECG shows a regular rhythm with a rate of 50 bpm. No P waves are seen before or after any QRS complex. The QRS complex duration is increased (0.18 sec). There appears to be a slurred upstroke of the QRS complex (↑), accounting for the widening of the QRS complex at the base, while the top of the QRS complex is narrower.
The QT/QTc intervals are prolonged (500/460 msec) but they are normal when the prolonged QRS complex duration is considered (420/390 msec). The QRS complex has a normal axis between 0° and +90° (positive QRS complex in leads I and aVF).
Noted is positive concordance, ie, tall R waves across the precordium from V1–V6 (←). The QRS complex duration and morphology are consistent with either a ventricular complex or a Wolff-Parkinson-White (WPW) pattern. However, the absence of P wave makes WPW a less likely diagnosis.
The accessory pathway begins in the atrium, and a WPW pattern on the ECG can only be seen if there is initial atrial activity. While a slurred upstroke of the QRS complex, representing direct myocardial activation, may be seen with either a ventricular complex or a WPW pattern, a slurred upstroke primarily altering the initial portion of the QRS complex upstroke is more characteristic of a WPW pattern.
In this case, the slurred upstroke is known as a delta wave. This indicates that initial ventricular activation is directly through the ventricular myocardium and not the normal His-Purkinje system, while ventricular activation thereafter is via the normal His-Purkinje pathway. In contrast, all of ventricular activation is abnormal in a ventricular rhythm and the whole QRS complex would be wide and abnormal.