This article is an answer to the ECG Case 173
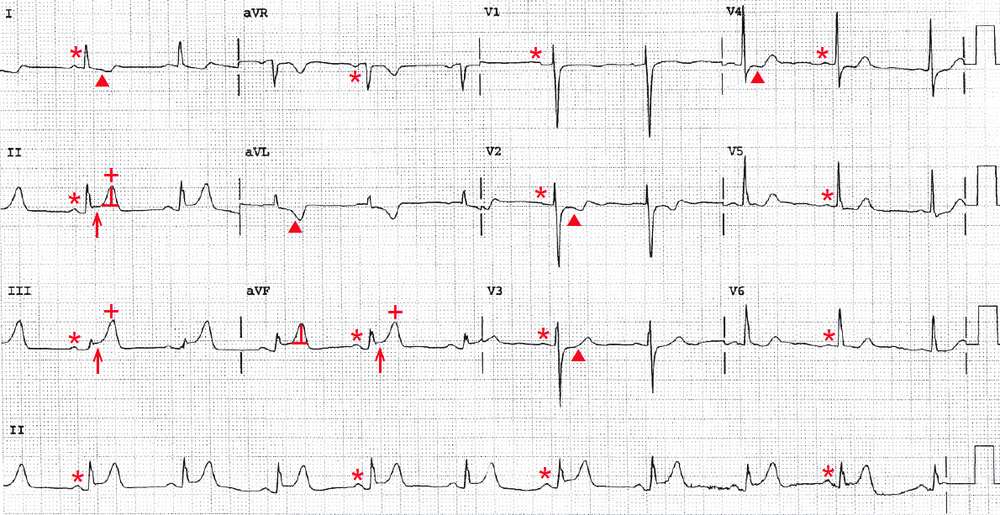
There is a regular rhythm at a rate of 60 bpm. There is a P wave (*) before each QRS complex with a stable PR interval (0.16 sec). The P wave is positive in leads I, II, aVF, and V4-V6 and negative in lead aVR.
This is a normal sinus rhythm. The T waves (+) are tall and symmetric in leads II, III, and aVF, and the ST segments (↑) are slightly elevated in these leads and have a normal concave morphology. This is an early acute inferior wall ST-segment elevation myocardial infarction (STEMI).
The ST segments (▲) in leads I, aVL, and V2-V4 are depressed and there is T-wave inversion, representing reciprocal changes. However, it is possible that the ST-segment changes in leads V2-V4 are the result of posterior wall involvement. A posterior wall MI can be confirmed by obtaining posterior leads V7-V8, placed under the left scapula.
This patient should undergo urgent reperfusion therapy. If he can be transferred within 90 minutes to a tertiary care center that has cardiac catheterization capability, he should undergo primary percutaneous coronary intervention. Otherwise, he should receive thrombolytic therapy.
Coronary angiography is likely to show occlusion of the right coronary artery (RCA), although an inferior MI can also be caused by occlusion of a dominant left circumflex coronary artery that supplies the posterior descending artery.
A clue to the culprit vessel is the relative degree of ST-segment elevation in leads II and III. If the degree of ST-segment elevation in lead III is greater than that in lead II, the artery most likely to be involved is the RCA. If the degree of ST-segment elevation in lead II is greater than that in lead III, the occlusion is more likely to be in a dominant circumflex artery. The left circumflex artery would most likely be the culprit vessel if there were a posterior wall MI.
- READ MORE: