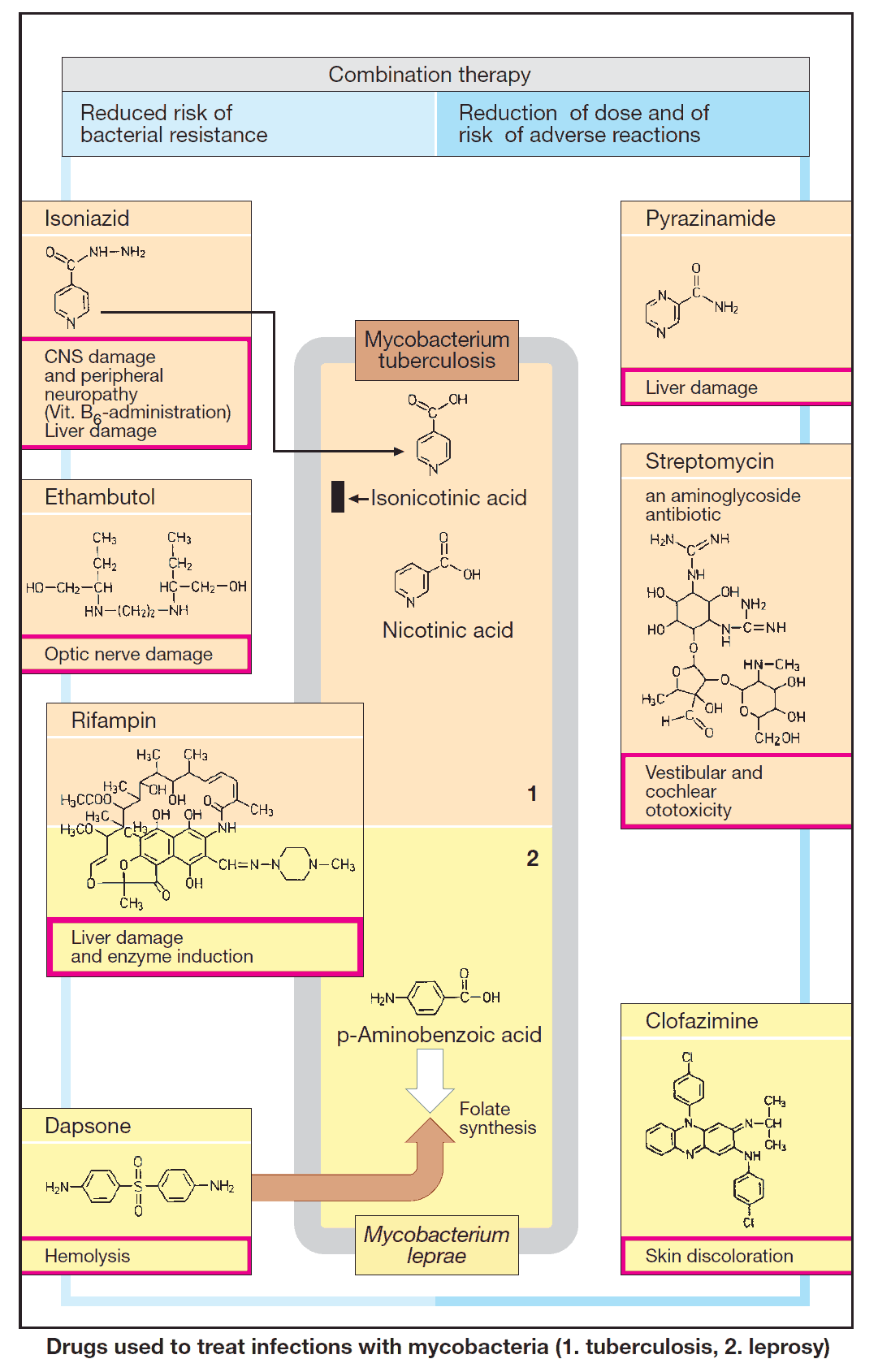
Drugs for Treating Mycobacterial Infections
The therapeutic principle applicable to both Tuberculosis and Leprosy is combined treatment with two or more drugs. Combination therapy prevents the emergence of resistant Mycobacteria and Mycobacterial Infections.