Table of Contents
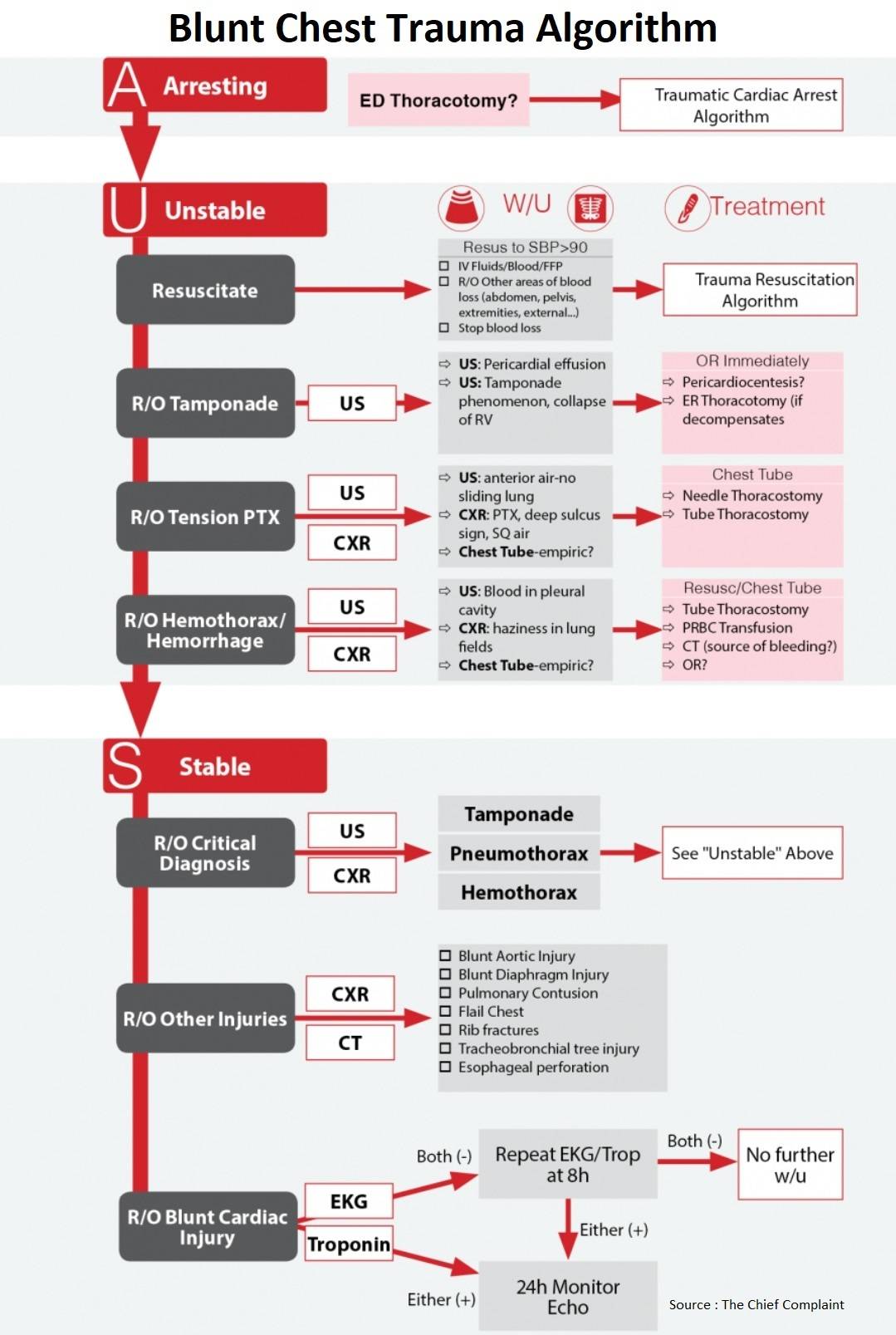
Cardiac Arrest from Blunt Chest Trauma
ED Thoracotomy indications:
- Trauma patient, CPR, no signs of life (SOL) +:
- Blunt trauma with CPR <10min
- Penetrating trauma with CPR <15min
- Penetrating trauma to neck/extremity < 5 min
No Signs of Life (SOL)
– No pulse
– No pupils
– No movement
– No breaths
– No PEA
– No cardiac motion (US)
- Resuscitative Thoracotomy (Open the left chest)
- Release tamponade and open resuscitation of heart ⇒ Control bleeding
- Open Cardiac Resuscitation
- Cross-clamp aorta → Shunt blood up
- Right Chest Tube
- Blood? → Clamshell thoracotomy to control bleeding
Survival rates:
- Overall survival rate 7.4%, dictated by location & mechanism of injury (J Am Coll Surg 2000;190:288- 98)
- Thoracic injury 10.7% (Cardiac-19.4%), abdominal injury 4.5%
- Penetrating injury 8.8% (stab wounds 17%, GSW 4.3%), blunt trauma 1.4%
Unstable Patient from Blunt Chest Trauma
1. Cardiac Tamponade
- Cause
- Blunt Cardiac Injury – Wall rupture,
- Coronary injury
- Clinical
- May be asymptomatic or non-specific
- Beck’s Triad: Distended neck veins, hypotension/shock, muffled hear sounds
Beck’s Triad
– Hypotension
– Distended neck veins
– Muffled heart sounds
- Diagnosis
- Bedside US: Pericardial effusion
- Sensitivity 100% for detections of pericardial effusion in multiple studies
- ECHO
- Bedside US: Pericardial effusion
- Treatment
- OR immediately for sternotomy
- ER thoracotomy if too unstable for OR
- Pericardiocentesis if unable to perform thoracotomy
- Closed chest CPR ineffective
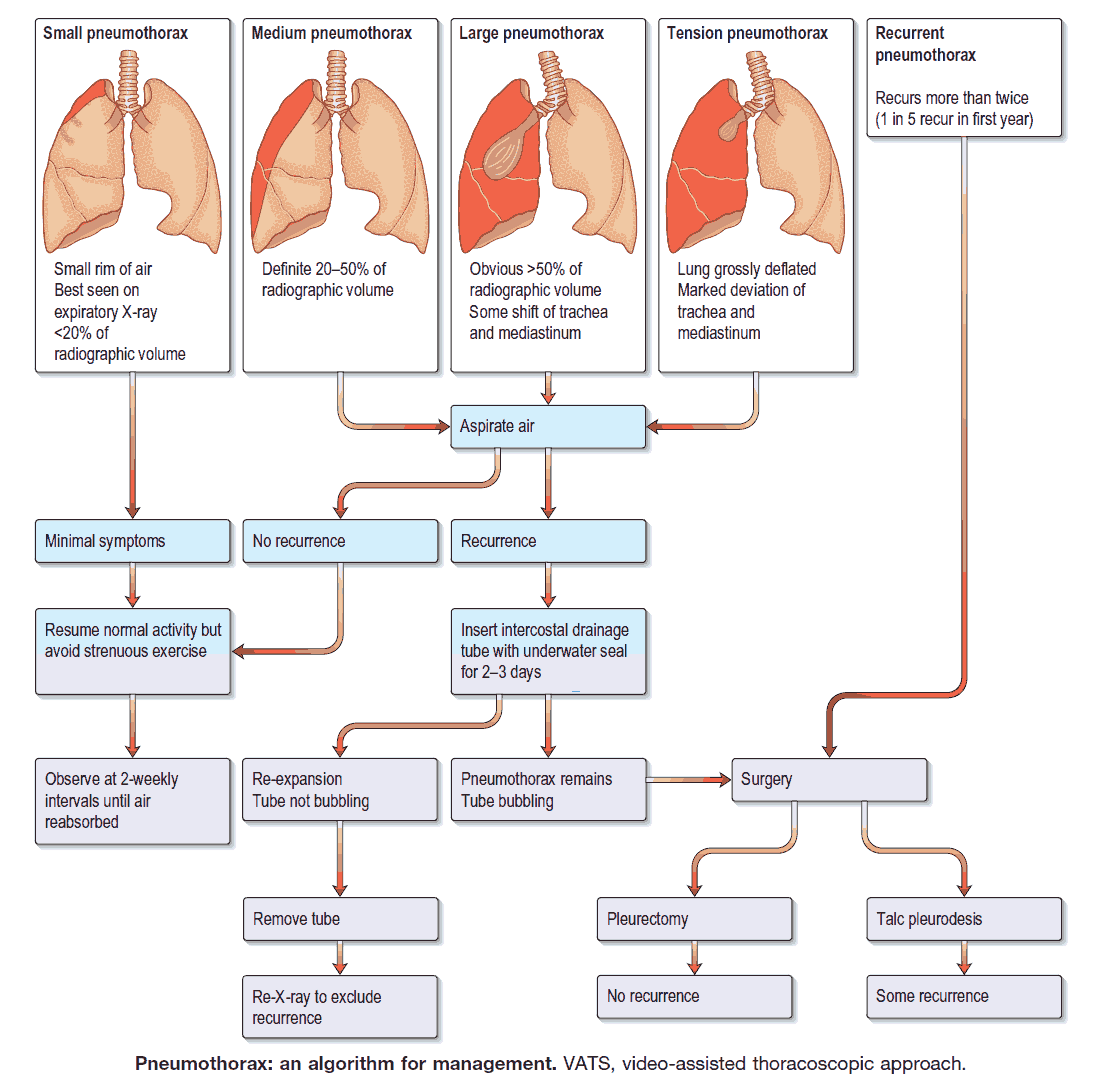
2. Pneumothorax
Clinical
- Often asymptomatic
- Dyspnea, tachypnea, absent breath sounds, poorly moving hemithorax, subcutaneous emphysema
Diagnosis
- Upright CXR
- PTX, deep sulcus sign, subcutaneous air
- Lung Ultrasound (Essentials 2013 #49)
- Diagnosis: Lung sliding, lung point
- True PTX? vs skin folds, blebs, peritoneal contents?
Treatment
- Chest tube: Unstable, hemothorax, multiple trauma
- Heimlich valve: stable, large Pneumothorax (>3cm)
- Observe & Oxygenate: stable, small-mod Pneumothorax (2-3cm; <20%)
- Occult Pneumothorax + Positive Pressure Ventilation (PPV) → if stable, can be observed
Chest Tube Stat!
– Traumatic cardiac arrest
– No BP/Pulse during resuscitation
– Hypotension + ↑ Ppeak or difficult to bag
– Hypotension or Hypoxia + decreased breath sounds or SQ emphysema
Tension Pneumothorax
Presentation:
- Classic presentation
- Respiratory distress
- Tachypnea
- Deviated trachea
- Hypotension/shock
- Unilateral decreased breath sounds
- The reality (Emerg Med J 2005;22:8–16)
- Tracheal deviation, hypoxia, and hypotension are inconsistent findings (<25% each)
- Course
- Hypoxia with progressive respiratory compromise → hypotension → cardiac failure, respiratory arrest
- Ventilated patients
- Sudden deterioration, hypoxia and hypotension (almost universal), increased Ppeak on vent, difficult to bag
Treatment: Tension Pneumothorax
- Needle decompression (inconsistent and unreliable)
- Immediate tube thoracostomy in mid-axillary line
Spontaneous Pneumothorax
Treatment
- ACCP recommends small bore (14F or smaller) catheter or 16-22 F chest tube connected to Heimlich valve or water seal
- If fails to re-expand → Chest tube
- May also do volume controlled re-expansion → Suction 200ml/hr from Heimlich and reclamp
Re-expansion pulmonary edema (mortality up to 20%)
- Risk factors: large size, long duration (>3days), rapid rate of re-expansion
- Clinical: 64% have symptoms within one hour, coughing, tachypnea, tachycardia and hypoxia
- Treatment: generally supportive, mechanical ventilation and hemodynamic support
Disposition: may discharge with Heimlich valve if lung fully expanded (large ptx should be admitted, observe 24h)
3. Hemothorax
Clinical
- Often asymptomatic
- Presentation: Dyspnea, tachypnea, hypovolemia, absent breath sounds, poorly moving hemithorax, dull on percussion
Diagnosis
- Upright CXR: 150-200ml needed in pleural cavity to diagnose hemothorax
- Supine CXR: Sensitivity of 40-60% in ruling out hemothorax
- US: Can diagnose as little as 20ml of blood; Sensitivity of 96%
Treatment
- Small Hemothorax
- Observation option: (J Trauma Acute Care Surg 2012;72(1):11)
- Consider as an option for small hemothorax (<300ml) but will likely need drainage
- Observation option: (J Trauma Acute Care Surg 2012;72(1):11)
- Significant Hemothorax
- Chest tube: Drainage of hemothorax
- Tube size doesn’t matter? (J Trauma Acute Care Surg 2012;72(2):422)
- Size of tube is not a factor in causing complications (28-32F is equivalent to 36-40F)
- Auto-transfusion for large hemothorax
- Antibiotics prior to tube insertion (Cefazolin 2g IV)
- Unstable/Life threatening bleed
- Urgent thoracotomy: (J Trauma 2011;70(2):510)
- More than 1,500 ml of blood immediately evacuated by tube thoracostomy
- Persistent bleeding from the chest, defined as 150 ml/h to 200 ml/h for 2 hours to 4 hours
- Persistent blood transfusion is required to maintain hemodynamic stability
- Clinical stability of patient should determine whether or not patient needs OR (persistent shock etc…)
- Urgent thoracotomy: (J Trauma 2011;70(2):510)
Complications
- Empyema – infection of retained hemothorax
- Retained fibrothorax – trapped lung
- Both may necessitate open thoracotomy and decortication
Stable Patint with Blunt Chest Trauma
1. Blunt Aortic Inury
- Epidemiology:
- Over 80% of patients die on scene
- Mechanism:
- Rapid deceleration from high speed MVA, falls from height >3m, ejection from vehicle/motorcycle, crush between two objects
- Evaluation
- All patients with significant mechanism of injury should have CT of mediastinum irrespective of CXR findings
- CXR: not sensitive to rule out aortic injury
- CT Chest: Normal CT essentially rules out aortic injury (J Trauma 1998;45(5):922)
- CT angiogram: sensitivity and NPV of approx 100%
- TEE: consider for patients too unstable for CT
- Treatment:
- Resuscitation
- Maintain low SBP <90 (β-blockers)
- Emergent surgical consultation
Blunt Aortic Inury CXR Findings
– Widened mediastinum (>8cm)
– Apical capping
– Depressed L mainstem bronchus
– Widened L paratracheal stripe
– Loss of aortic knob contour
– Deviated NG tube
2. Blunt Cardiac Injury
Spectrum
- Structural Wall contusion (rarely clinically significant)
- Wall rupture (die at scene)
- Incidence 0.045%, Mortality 89% (J Trauma. 2009;67(4):788)
- Septal rupture (die at scene)
- Valve disruption (die at scene)
- Coronary injury (die at scene)
- Conclusion: Clinically significant structural injuries very rare in survivors
- Wall rupture (die at scene)
- Electrical: Arrhythmias (Crit Care Clin 2004;20:57–70)
- Non-specific changes (50-70%):
- Sinus tachycardia/bradycardia, PAC/PVC, conduction delays, ST-T wave changes
- Atrial arrhythmias (4-30%)
- Atrial fibrillation most common arrhythmia to require treatment
- Ventricular arrhythmias (2-10%)
- Non-specific changes (50-70%):
Blunt Cardiac Injury Spectrum
□ Free wall rupture
□ Septal rupture
□ Coronary artery injury
□ Cardiac failure
□ Complex arrhythmias
□ Minor EKG/cardiac enzyme abnormalities
Who is at risk?
- All patients with severe chest injury
- High risk mechanism: high speed, rapid deceleration, airbag, steering wheel damage, seatbelt restraint
- Associated chest trauma: fracture, contusion, hemothorax/pneumothorax
Evaluation:
- Controversial: many approaches to rule out Blunt Cardiac Injury
- Serial troponin/EKG (J Trauma 2003;54:45-51)
- Serial EKG/Trop at 0 and 8 hours → sensitivity 100%
- If either positive → rule out ACS, 24h monitoring for arrhythmias, TTE
- If all normal, can discharge home
3. Blunt Diaphragmatic Rupture
General:
- 50-80% on left side, right side rupture associated with liver injury (50%)
- Clinical symptoms are varied, subtle and non-specific
- Other injuries? Isolated diaphragm injuries from blunt trauma are rare
Mechanism
- Severe abdominal trauma → sudden, major increase of intra-abdominal pressure (MVC) → weak parts of diaphragm pull apart → +/- translocation of abdominal contents
Diagnosis:
- CXR
- Classic: bowel in chest wall (<50% translocation), elevated hemidiaphragm, displaced NG tube, box-like R hemidiaphragm
- Usual: abnormal but non-specific
- CT → high specificity, sensitivity still low
- Collar sign on CT: Constriction of colon/stomach passing through tear
- If high clinical suspicion, may need surgical evaluation
- Delayed presentation:
- Most diaphragmatic ruptures missed on initial trauma eval → present later with bowel obstruction/incarceration
4. Tracheobronchial Tree Injury
Upper Airway Injury
- Usually straightforward diagnosis
- Treatment: Relieve obstruction and secure definitive airway
Lower Airway Injury
- Clinical Presentation
- Rare and can be subtle (depending on size of defect, air leak, pleural communication)
- Small defect:
- Mediastinal air on CT, subcutaneous emphysema, hemoptysis
- Large defect:
- Dyspnea, Pneumothorax, Persistent Pneumothorax after chest tube, air leak after chest tube
- May need 2nd chest tube
- Diagnosis
- CT
- Difficult to ID on CT → usually within 2cm of carina (right mainstem bronchus or trachea)
- Bronchoscopy
- Locate injury to advance ETT beyond site of injury, possibly to unaffected mainstem bronchus
- Diagnose location and size of injury → surgical repair
- CT
- Treatment
- High mortality from ventilation/oxygenation compromise
- Thoracic Surgery for repair
5. Pulmonary Contusion
Mechanism
- High-energy mechanisms of trauma with rapid deceleration, compression, shear, or inertial forces
- MVC, falls from great heights, blast injuries
Pathophysiology
- Lung parenchyma damage → alveoli filled with mucus and fluid → decreased compliance, decreased oxygen diffusion, ventilation-perfusion mismatch, and shunting
Clinical
- May be asymptomatic
- SOB (dyspnea), hypoxia and increased work of breathing proportional to the degree of contused lung
- Symptoms progress over hours and usually peak at 72h
Diagnosis
- CXR
- Classical: infiltrates or consolidation
- Normal CXR in 50% pts on arrival → then progress to classic CXR at 24h
- CT scan
- More sensitive than CXR → may have parenchymal changes on CT with normal CXR
Treatment
- Mostly supportive
- Oxygen, pulmonary toilet, ICU monitoring
- Avoid over-hydration → may worsen lung edema
- NPPV may help avoid intubation in selected patients
- Intubation and PPV if other modalities fail
- Goal: optimize oxygenation while minimizing further lung trauma
- Low Vt (6ml/kg) and maintain low Ppl <30
6. Flail Chest
- Cause
- Anterior or lateral double fractures of 3 or more adjacent ribs
- Flail segment moves in during inspiration
- Diagnosis
- CXR
- Chest CT – in severe trauma to evaluate for pulmonary contusion or other associated injuries
- Treatment
- Continuous pulse oximetry/ABG
- Analgesia
- Mechanical ventilation for severe trauma
7. Rib Fractures
- Diagnosis
- CXR (costochondral junction fractures may not be seen)
- Treatment
- Mild-moderate pain: oral analgesics
- Severe pain: IV pain medication or epidural
- Incentive spirometry
- Associated injuries
- Pneumothorax / hemothorax
- 1st three ribs: subclavian vessels or major bronchi
- Pulmonary contusion / Blunt Cardiac Injury / Aortic rupture / Diaphragm rupture
Read Also : Penetrating Chest Trauma Algorithm
References
- McGillicuddy D, Rosen P. Diagnostic dilemmas and current controversies in blunt chest trauma. Emerg Med Clin North Am. 2007 Aug;25(3):695-711, viii-ix. doi: 10.1016/j.emc.2007.06.004. PMID: 17826213.
- Rhee PM, Acosta J, Bridgeman A, Wang D, Jordan M, Rich N. Survival after emergency department thoracotomy: review of published data from the past 25 years. J Am Coll Surg. 2000 Mar;190(3):288-98. doi: 10.1016/s1072-7515(99)00233-1. PMID: 10703853.
- Leigh-Smith S, Harris T. Tension pneumothorax—time for a re-think? Emergency Medicine Journal 2005;22:8-16.
- Baumann MH, Strange C, Heffner JE, Light R, Kirby TJ, Klein J, Luketich JD, Panacek EA, Sahn SA; AACP Pneumothorax Consensus Group. Management of spontaneous pneumothorax: an American College of Chest Physicians Delphi consensus statement. Chest. 2001 Feb;119(2):590-602. doi: 10.1378/chest.119.2.590. PMID: 11171742.
- Inaba K, Lustenberger T, Recinos G, Georgiou C, Velmahos GC, Brown C, Salim A, Demetriades D, Rhee P. Does size matter? A prospective analysis of 28-32 versus 36-40 French chest tube size in trauma. J Trauma Acute Care Surg. 2012 Feb;72(2):422-7. doi: 10.1097/TA.0b013e3182452444. PMID: 22327984.
- Mowery NT, Gunter OL, Collier BR, Diaz JJ Jr, Haut E, Hildreth A, Holevar M, Mayberry J, Streib E. Practice management guidelines for management of hemothorax and occult pneumothorax. J Trauma. 2011 Feb;70(2):510-8. doi: 10.1097/TA.0b013e31820b5c31. PMID: 21307755.
- Mirvis SE, Shanmuganathan K, Buell J, Rodriguez A. Use of spiral computed tomography for the assessment of blunt trauma patients with potential aortic injury. J Trauma. 1998 Nov;45(5):922-30. doi: 10.1097/00005373-199811000-00014. PMID: 9820704.
- Teixeira PG, Inaba K, Oncel D, DuBose J, Chan L, Rhee P, Salim A, Browder T, Brown C, Demetriades D. Blunt cardiac rupture: a 5-year NTDB analysis. J Trauma. 2009 Oct;67(4):788-91. doi: 10.1097/TA.0b013e3181825bd8. PMID: 19680160.
- Schultz JM, Trunkey DD. Blunt cardiac injury. Crit Care Clin. 2004 Jan;20(1):57-70. doi: 10.1016/s0749-0704(03)00092-7. PMID: 14979329.
- Velmahos, George C. MD; Karaiskakis, Marios MD; Salim, Ali MD; Toutouzas, Konstantinos G. MD; Murray, James MD; Asensio, Juan MD; Demetriades, Demetrios MD, PhD. Normal Electrocardiography and Serum Troponin I Levels Preclude the Presence of Clinically Significant Blunt Cardiac Injury. The Journal of Trauma: Injury, Infection, and Critical Care 54(1):p 45-51, January 2003.