Table of Contents
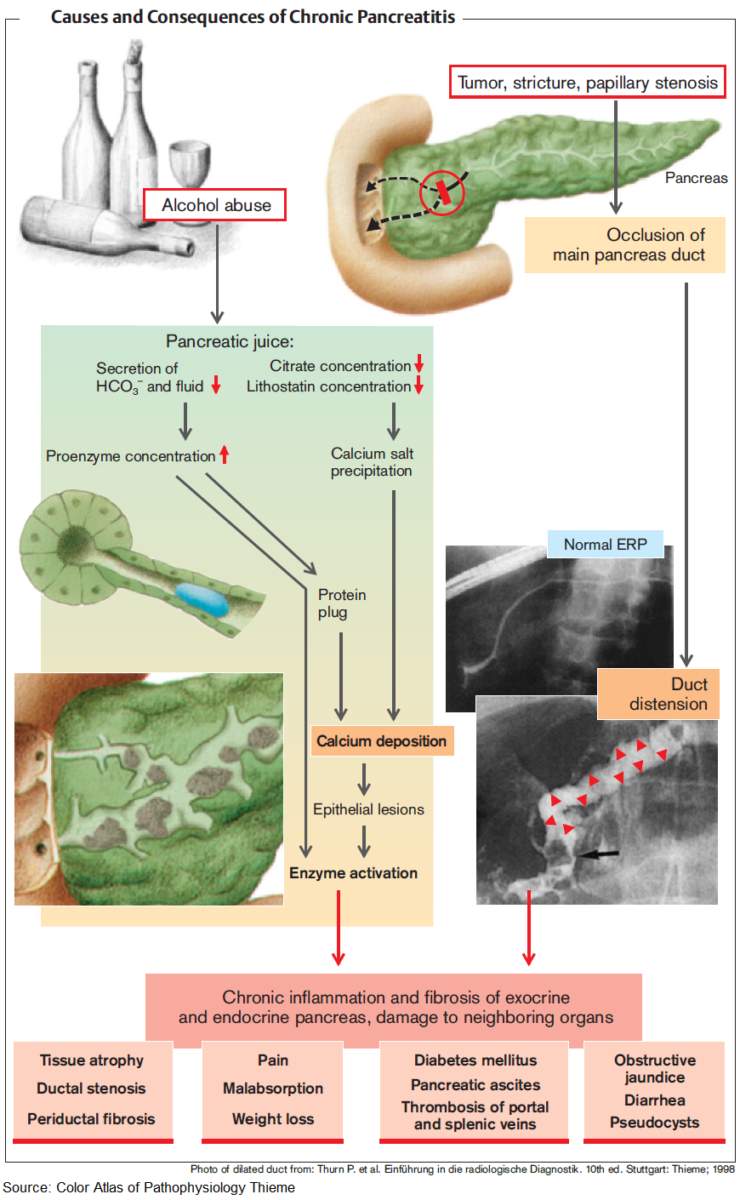
Chronic pancreatitis occurs when there is irreversible and progressive destruction of the pancreas.
Etiology of the Pain in Chronic Pancreatitis
While the etiology of the pain in chronic pancreatitis is not well understood, it is most likely due to:
- chronic inflammation
- altered nociception
- tissue ischemia
Symptoms and Signs of Chronic Pancreatitis
Patients frequently present with disabling chronic abdominal pain with those with intractable pain requiring large doses of pain medications.
Due to the loss of pancreatic function, patients may experience:
- steatorrhea
- malabsorption
- weight loss
- anorexia
- nausea
- vomiting
- diabetes mellitus
The transition from acute to chronic pancreatitis can be indistinct and difficult to discern. Moreover, the clinical picture of chronic pancreatitis can be highly variable.
Clinicians frequently feel conflicted about doing a detailed workup as many of these patients are frequent users of the emergency department (ED) and may have opioid dependency issues. Nonetheless, it is important to assess a patient’s abdominal pain, as well as for complications of chronic pancreatitis.
Chronic Pancreatitis: Investigations and Diagnosis
In a patient with acute pancreatitis, lipase levels will most frequently be elevated. These enzymes levels can normalize as the disease progresses. In chronic pancreatitis, clinicians may be falsely reassured when they see a normal lipase, despite true pancreatic functional burnout.
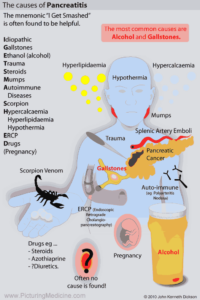
Further, patients who do not consume any alcohol and present with chronic pancreatitis should be screened for gallstones and other toxic-metabolic, autoimmune, and genetic etiologies.
To confirm the diagnosis in those with suspicious presentations, abdominal CT or MRI may be used to image the pancreas.
In some cases, patients may need referral for an endoscopic ultrasound (EUS) or magnetic resonance cholangiopancreatography (MRCP), especially for mild or early disease states.
Once a diagnosis is established, however, repeated imaging on subsequent presentations to the ED is not necessarily indicated.
Complications of Chronic Pancreatitis as the Cause of Pain and Acute Exacerbation
While it may be easy to dismiss patients with chronic pancreatitis as “opiate seeking,” it is important to consider whether complications of this disease may be contributing to their acute exacerbation.
For example, are there any new features, such as a change in the nature of the pain? Is a fever present? Patients with intractable vomiting, or who are unable to tolerate any food or fluids, may require further evaluation.
Complications of Chronic Pancreatitis include:
- Strictures of the pancreatic ducts
- Pseudocysts
- Pancreatic stones
- Fistulization
- Abscess
- Fluid collections and pancreatic necrosis (can develop into infections or abscesses that require antibiotics or drainage)
- Diabetes mellitus (Secondary to a loss of islet cells, can manifest in the later stages of disease. These patients may develop neuropathy and retinopathy and rarely, may even develop diabetes ketoacidosis)
- Pancreatic cancer (especially in patients with hereditary pancreatitis)
Management of the Pain in Chronic Pancreatitis
The ED management of pancreatic pain can be very challenging as therapeutic options may be limited.
1. Medications
- Acetaminophen is considered to be a firstline therapy, but by the time these patients arrive to the ED, they may require or request opioid medications.
- Nonsteroidal anti-inflammatory drugs (NSAIDs).
- Neuropathic pain modulators such as antidepressants (e.g., cyclic antidepressants and serotonin reuptake inhibitors), as well as, gabapentin. All have been shown to be effective.
- Ketamine (oral and intravenous) – more recently, some success has been demonstrated with the use ketamine, and this agent continues to be studied.
- Corticosteroid therapy for those with autoimmune disease can be beneficial.
2. Lifestyle Changes
Harm reduction counseling is extremely important.
- Alcohol abstinence has been shown to slow or halt disease progression, which may improve chronic pancreatic pain.
- Cigarette smoking is also a major risk factor and contributor to the morbidity of chronic pancreatitis.
- Eating smaller, low-fat meals.
- Adding a proton pump inhibitor.
- Pancreatic enzymes and micronutrient supplementation to improve digestion.
In patients with intractable chronic pancreatic pain, referral for a celiac nerve block, endoscopy, or surgery should be considered.
3. Celiac Nerve Block
4. Endoscopy
- Ductal decompression
- Lithotripsy
- Sphincterectomy
5. Surgery
- Pancreatectomy
- Islet cell transplantation
Key Points
- Lipase levels may be normal, despite true functional pancreatic burnout.
- Remember to assess patients for complications if the chronic pancreatic pain cannot be controlled. These include pancreatic pseudocyst, necrosis, stricture, and abscess.
- If complications are not present and the chronic pancreatic pain is not well controlled, consider referring patients for specialist consultation with a gastroenterologist, surgeon, or pain management specialist.
References / Suggested Readings
- Braganza JM. Chronic pancreatitis. Lancet. 2011;377:1184–1197.
- Nair RJ. Chronic pancreatitis. Am Fam Physician. 2007;76:1679–1688.
- Ahmed SA. Chronic pancreatitis: Recent advances and ongoing challenges. Curr Probl Surg. 2006;43:127–238.
- Puylaert M. Pain in chronic pancreatitis. Pain Pract. 2011;11:492–505.
- Juel J. Study protocol for a randomised, double-blinded, placebo-controlled, clinical trial of S-ketamine for pain treatment in patients with chronic pancreatitis (RESET trial). BMJ Open. 2015;5:e007087.
- Chauhan S. Pain management in chronic pancreatitis: A treatment algorithm. Best Pract Res Clin Gastroenterol. 2010;24:323–335.