Table of Contents
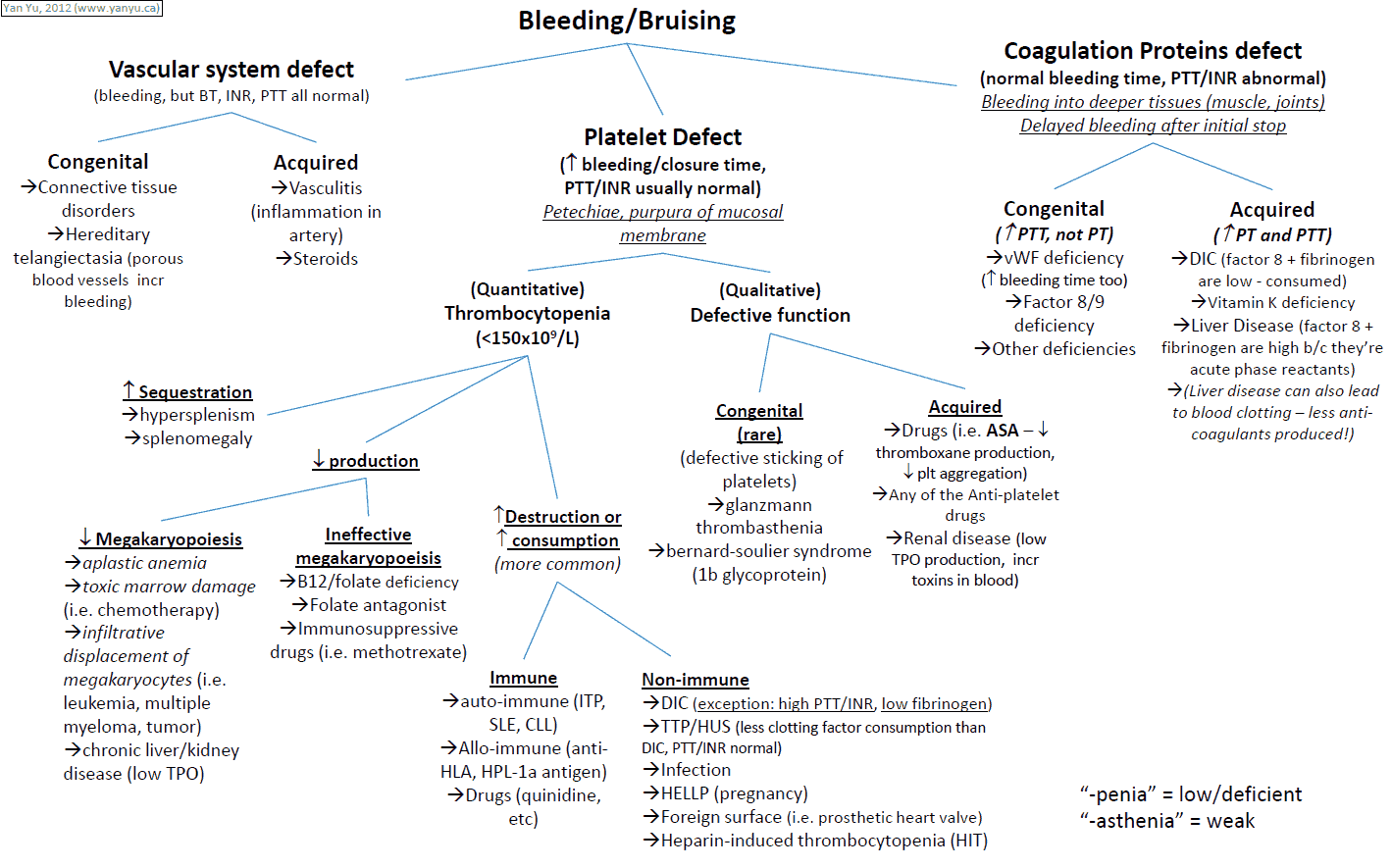
Bruising and bleeding arise when there is abnormal hemostasis. Hemostasis is dependent on normal platelet number and function, an intact coagulation pathway, and normal vessel walls.
Differential Diagnosis of Bleeding and Bruising
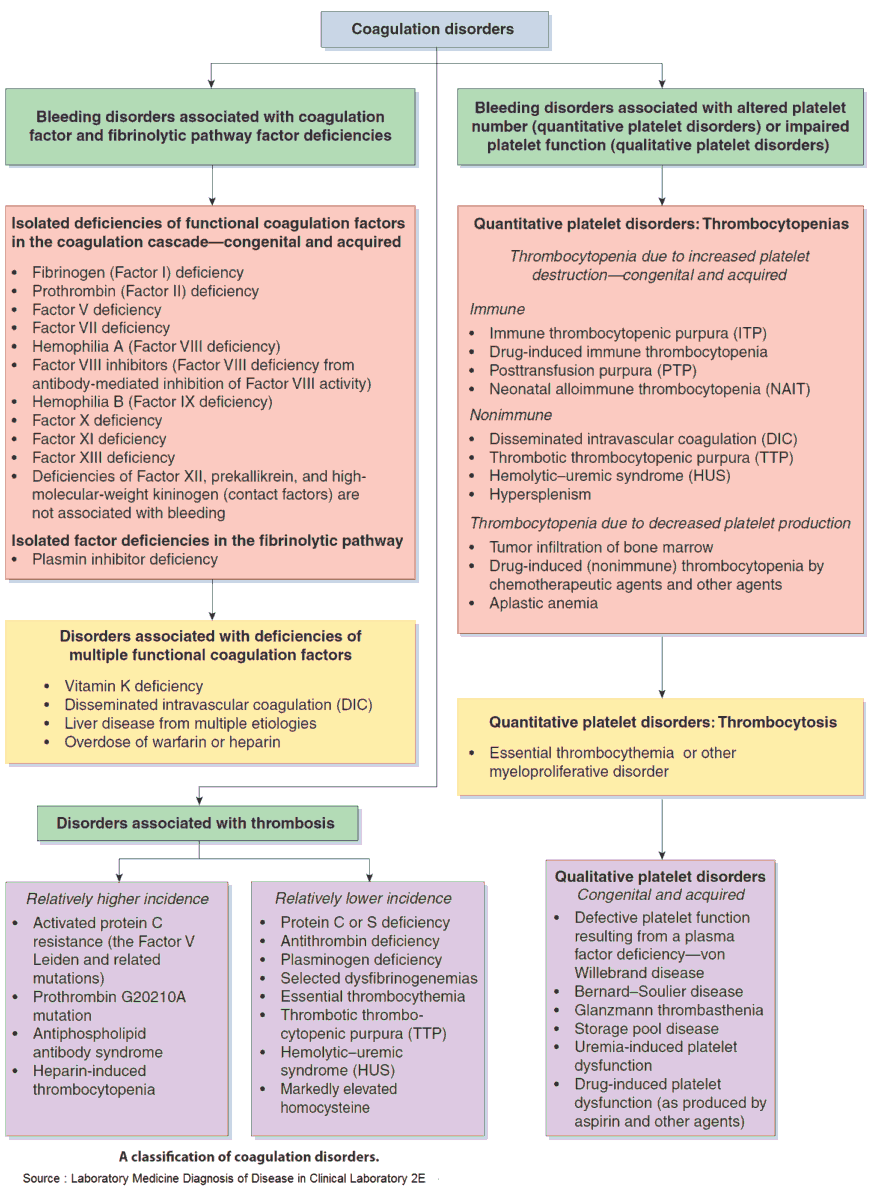
1. Platelet abnormalities
Platelets may be reduced in number or function.
Thrombocytopenia
- Reduced production:
- bone marrow failure
- drugs (cotrimoxazole)
- postchemotherapy or postradiotherapy
- human immunodeficiency virus (HIV)
- EBV infection
- hepatitis
- Increased consumption:
- disseminated intravascular coagulation
- thrombotic thrombocytopenic purpura
- autoimmune disease
- systematic lupus erythematosis (SLE)
- Abnormal distribution: splenic pooling in splenomegaly
- Dilutional: massive transfusion
Platelet dysfunction
- Hereditary: Glanzmann’s thrombasthenia.
- Acquired: aspirin, heparin, uremia.
2. Coagulation Abnormalities
Coagulopathies may be due to vitamin K deficiency or specific factor deficiency.
Factor deficiency
- Hereditary: hemophilia A (factor VIII), hemophilia B (factor IX), von Willebrand’s factor.
- Acquired: liver disease.
Vitamin K deficiency
Factors II, VII, IX, and X are dependent on vitamin K. Deficiency may be caused by:
- Malabsorption: bowel pathology such as celiac disease or biliary obstruction (vitamin K is fat-soluble).
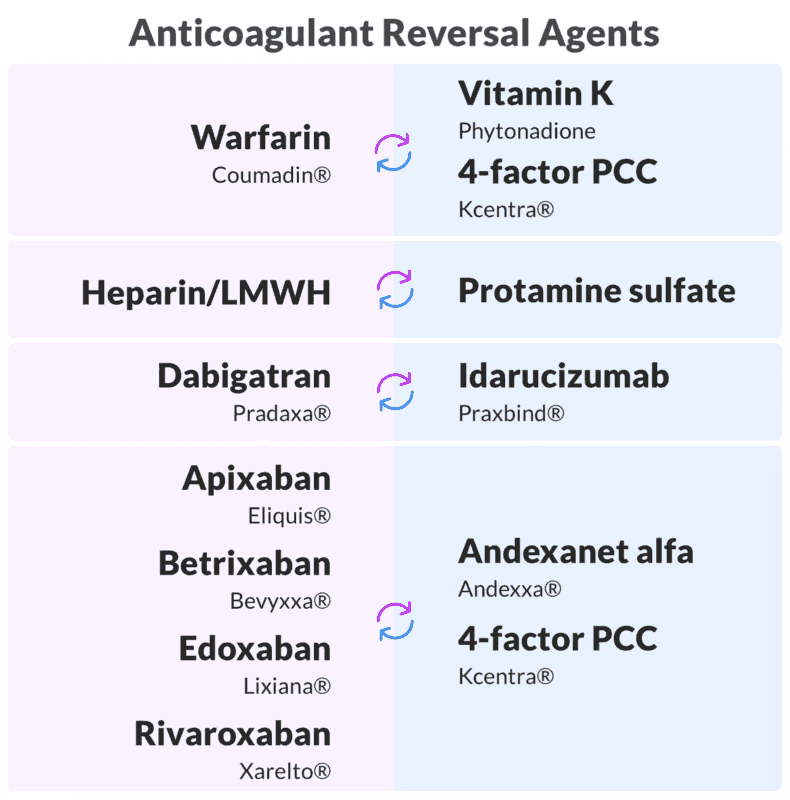
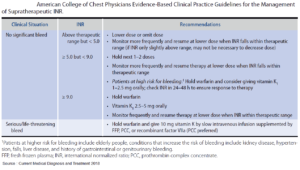
- Antagonist drugs: coumarins (warfarin).
3. Vessel wall abnormalities
Vessel wall abnormalities may be inherited or acquired.
Hereditary: Hereditary hemorrhagic telangiectasia.
Acquired
- Trauma.
- Physiologic: senile purpura.
- Drugs: corticosteroids.
- Infections: meningococcal septicemia.
- Vitamin deficiency: scurvy (vitamin C).
- Connective tissue disease: pseudoxanthoma elasticum, Ehlers-Danlos syndrome.
- Endocrine: Cushing’s syndrome.
History and Symptoms in the Patient with Bleeding and Bruising
The history should focus on three areas.
- What is the pattern and extent of the bleeding and bruising?
- Are there any clues as to the possible underlying cause?
- Have complications occurred?
1. What is the pattern and extent of bleeding and bruising?
- Platelet abnormalities (low number or dysfunction) cause skin or mucosal purpura and hemorrhage, with prolonged bleeding following trauma or surgery.
- Vessel wall abnormalities cause petechiae and ecchymoses due to bleeding from small vessels, mostly in the skin, but occasionally in mucous membranes.
- Coagulopathies cause hemarthroses, muscle hematomas, postoperative or traumatic bleeding, and mucosal bleeding (von Willebrand’s disease).
2. What is the underlying cause?
- Bleeding and bruising: “normal” and related to recent trauma or due to an underlying hemostatic abnormality.
- Age: senile purpura seen mostly on the upper limbs.
- Abdominal symptoms: celiac disease, gallstones, liver disease.
- Drug history: aspirin, heparin, warfarin, steroids, previous chemotherapy.
- Family history: hemophilia, hereditary hemorrhagic telangiectasia.
- Symptoms of meningitis: meningococcal sepsis.
- Hyperextensibility of the skin or joints: Ehlers-Danlos syndrome, pseudoxanthoma elasticum.
- Poor diet: scurvy (ecchymoses predominantly on the lower limbs).
- Known acquired immune deficiency syndrome or risk factors for HIV infection.
3. Have complications occurred?
- Symptoms of anemia
- Symptoms of shock
- Muscle pain or mass
- Joint pain or deformity
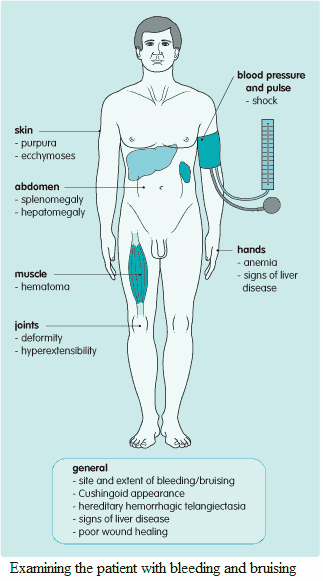
Examination and Signs in the Patient with Bleeding and Bruising
1. What is the pattern and extent of bleeding and bruising?
The sites and types of lesions should be documented (see above). “Purpura” includes petechiae (small pinpoint bleeds into the skin) and ecchymoses (small bruises).
2. How severe has the bleeding been?
Shock should be looked for urgently in the sick patient by measuring pulse and blood pressure; signs of anemia should also be sought. Finally, look for joint deformities or a mass in muscle.
3. Are there signs suggestive of specific diseases?
- Signs of liver disease.
- Splenomegaly (whatever cause): platelet pooling.
- Cushingoid appearance: steroid therapy, endocrinopathy.
- Hereditary hemorrhagic telangiectasia: characteristic petechiae on the tongue and lips.
- Meningism.
- Scurvy: corkscrew hairs with hyperkeratosis of the follicles, perifollicular hemorrhages, gum hypertrophy, poor wound healing.
- Ehlers-Danlos syndrome: hyperextensible skin and joints, “fish-mouth” wounds, pseudotumors over the elbows and knees.
- Pseudoxanthoma elasticum: loose skin in neck, axillae, anticubital fossae and groins, “chicken skin,” blue sclera, angioid streaks in the retina, hyperextensible joints.
Thrombocytopenic purpura and vasculitic purpura may look identical, but the lesions in the latter are usually raised and may be tender.
Investigating and Diagnosing the Patient with Bleeding and Bruising
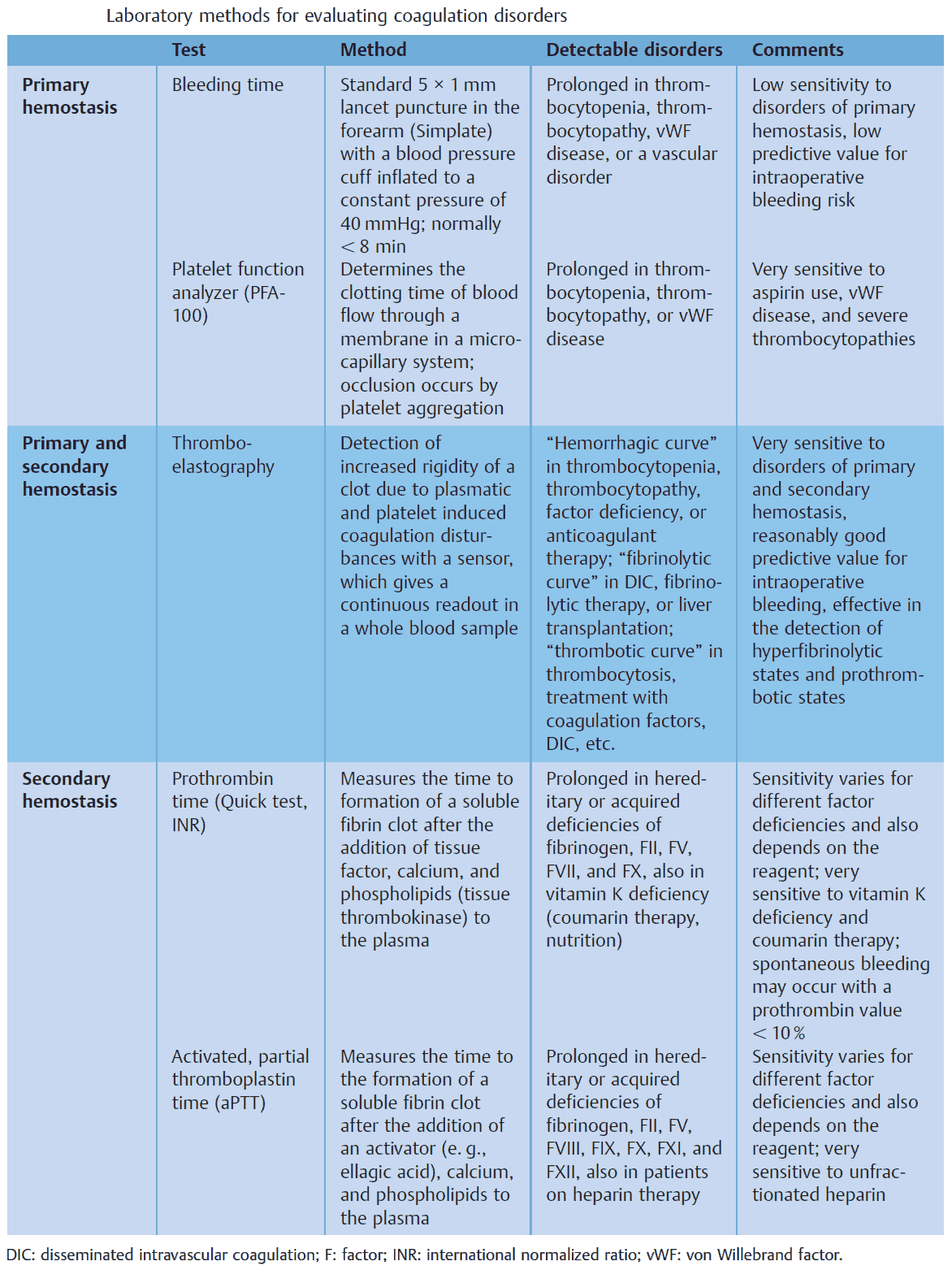
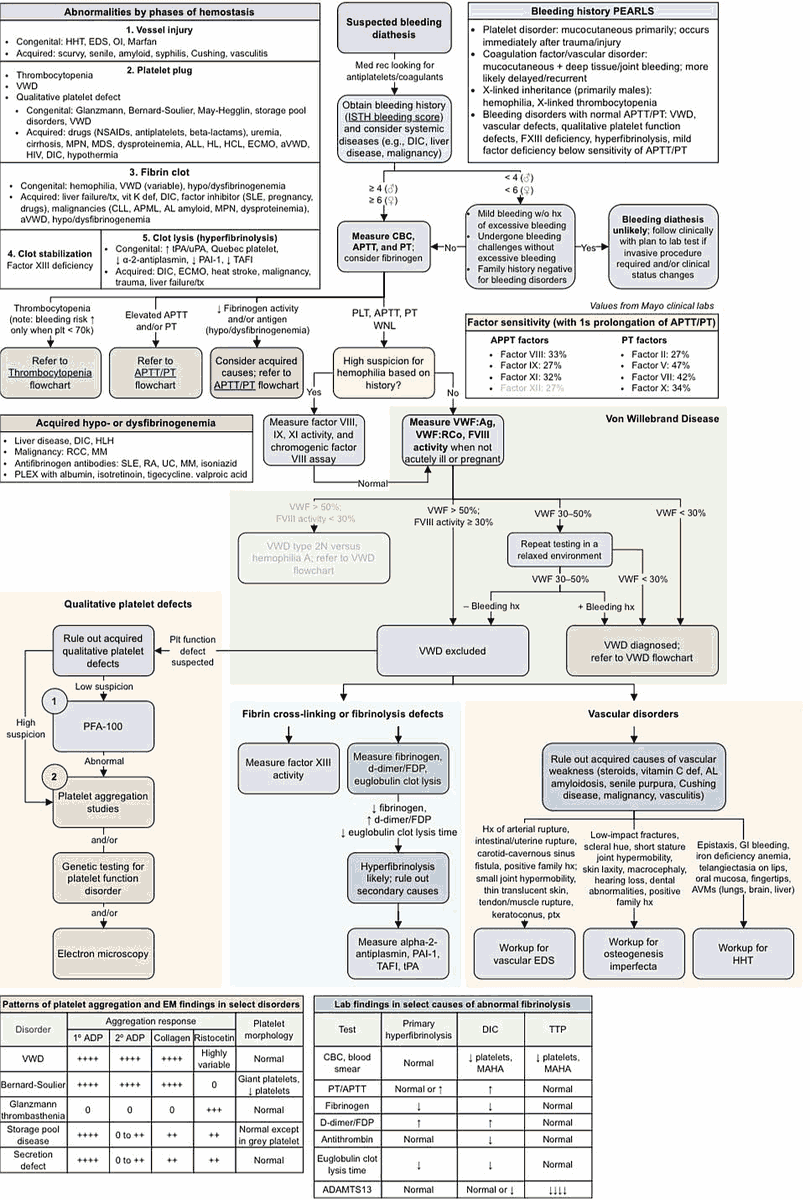
When an abnormality of hemostasis is suspected, a platelet count and simple coagulation assays should be performed. More specific tests to diagnose the underlying cause can then be considered.
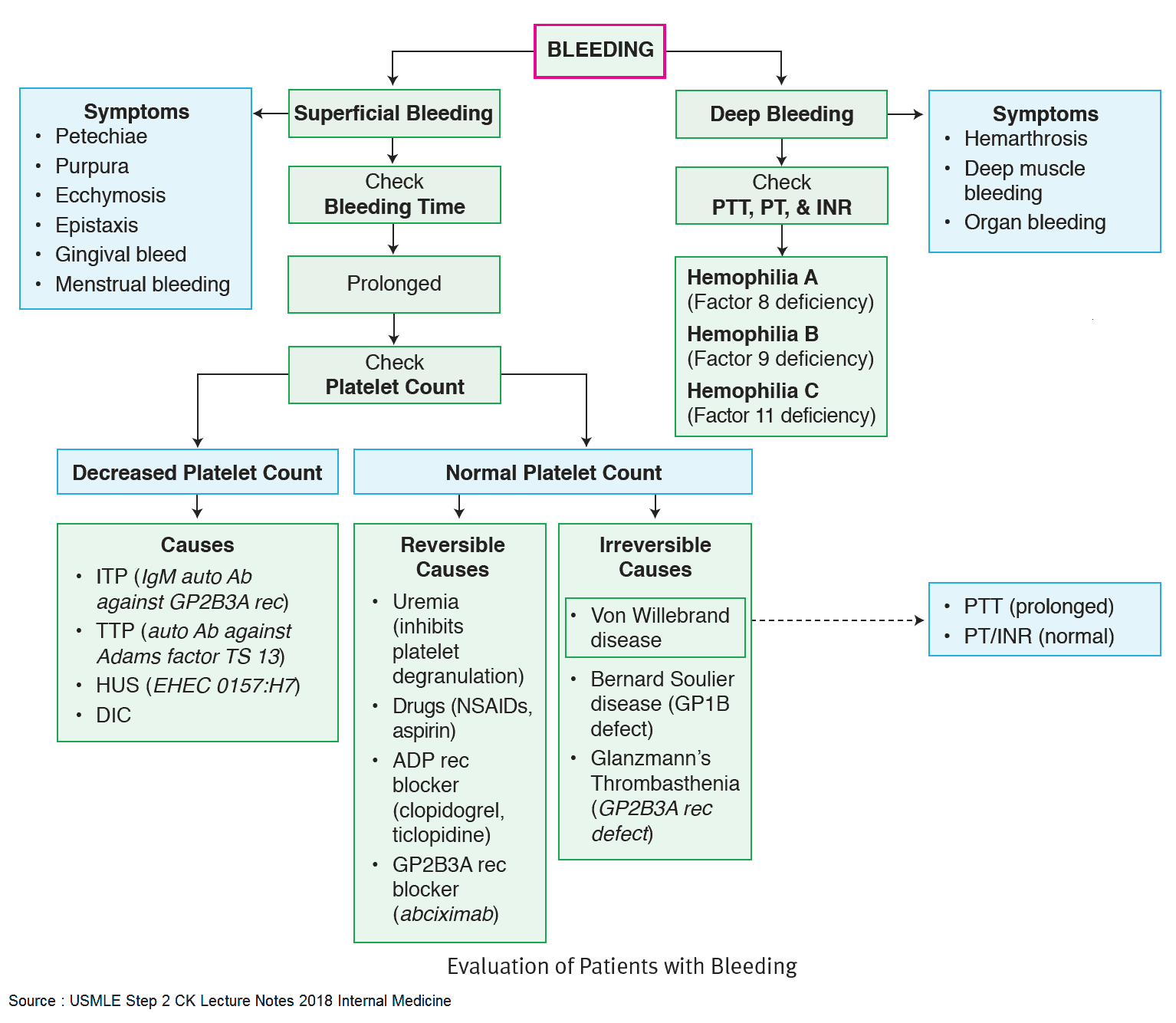
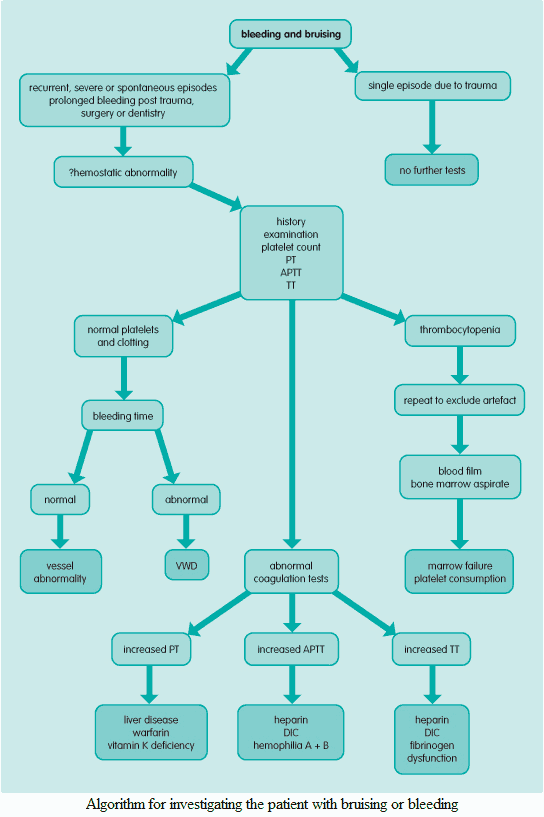
Platelet Count
If thrombocytopenia is present, request a peripheral blood smear (exclude artifactual result due to platelet clumping, look for acute leukemia or disseminated intravascular coagulation) and bone marrow aspirate (increased megakaryocytes in consumptive thrombocytopenia, e.g., idiopathic thrombocytopenic purpura or reduced megakaryocytes in bone marrow failure).
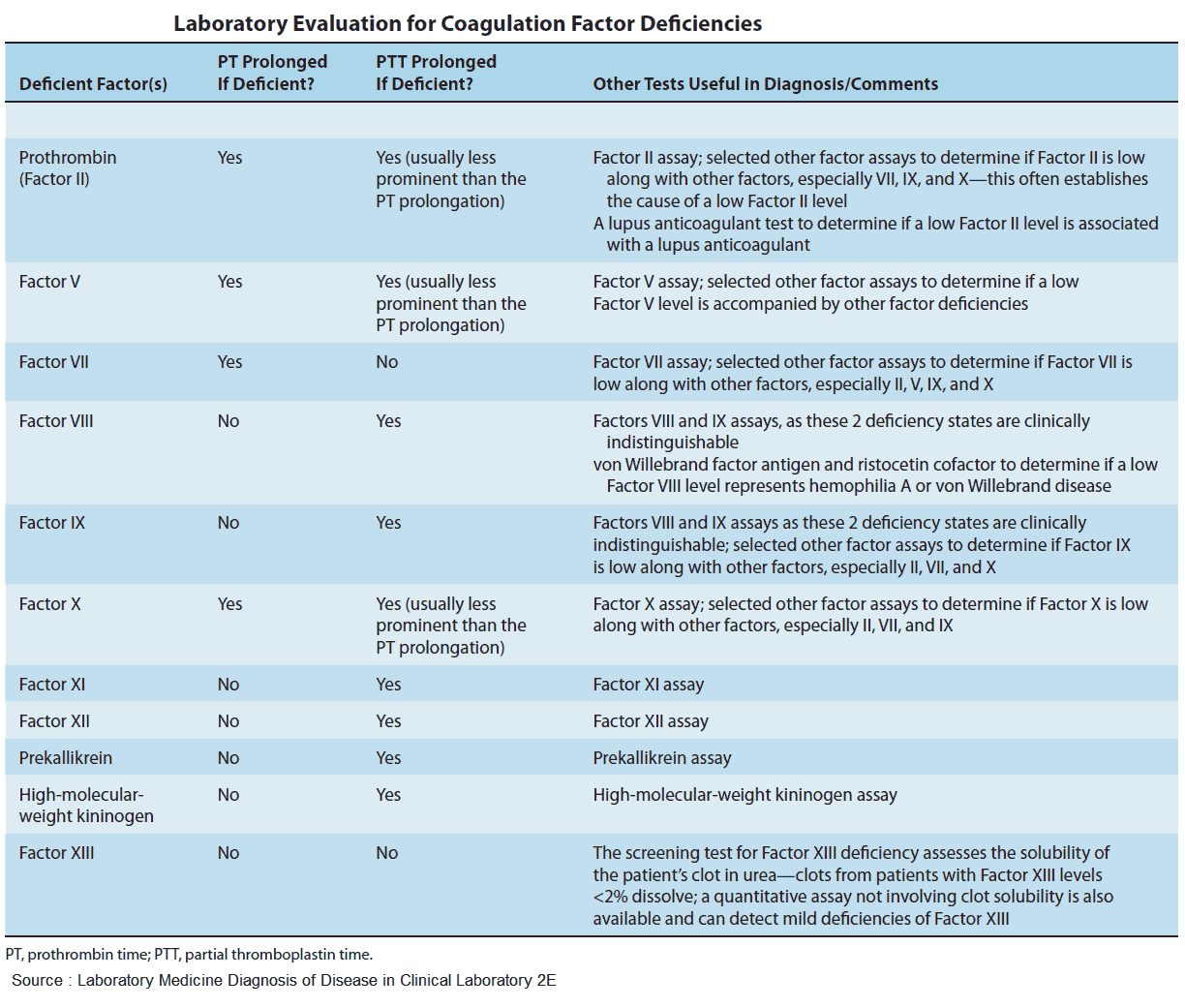
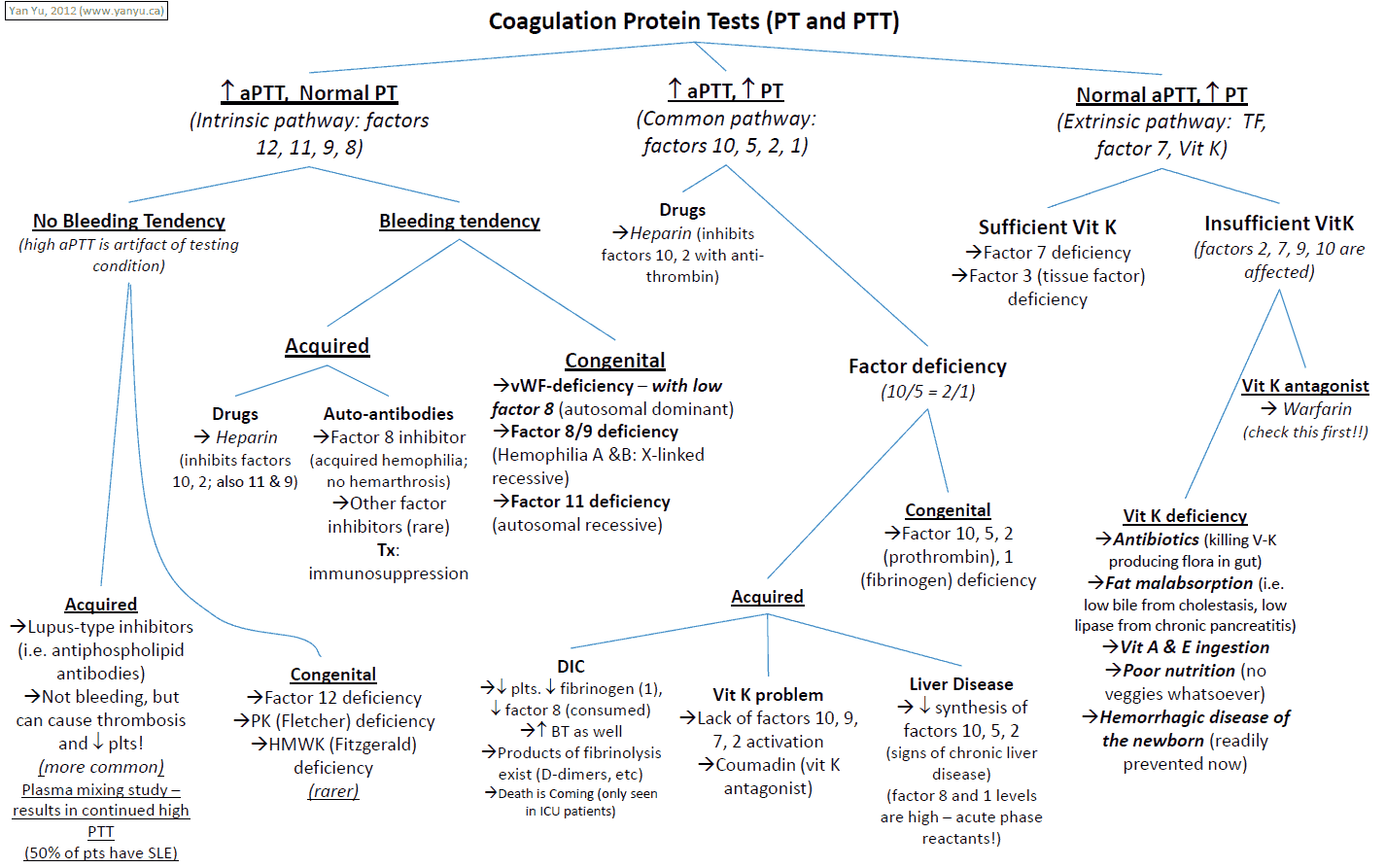
Prothrombin Time
Prothrombin time measures the extrinsic system (VII) and common pathway (X, V, prothrombin, and fibrinogen). It is prolonged in liver disease and warfarin therapy, and is generally expressed as international normalized ratio (INR).
Activated partial thromboplastin time or kaolin-cephalin clotting time
This measures the intrinsic system (XII, XI, IX, and VIII) and common pathway (X, V, prothrombin, and fibrinogen). It is prolonged in:
- heparin therapy
- factor deficiency such as factor VIII (hemophilia A) and factor IX (hemophilia B, Christmas disease)
- disseminated intravascular coagulation
- von Willebrand’s disease
Thrombin Time
Thrombin time measures the activity of thrombin and fibrinogen in the common pathway. It is prolonged in fibrinogen deficiency (disseminated intravascular coagulation) or fibrinogen dysfunction. Prolonged thrombin time may also result from heparin therapy (inhibition of thrombin activity).
Bleeding time (rarely performed)
Bleeding time measures platelet function. It is only performed if platelet count, coagulation screening tests (as above), peripheral blood smear, and bone marrow are normal. It is prolonged in aspirin therapy, uremia, and von Willebrand’s disease.
Fibrin degradation products and D-dimers
Fibrin degradation products and D-dimers will be elevated in disseminated intravascular coagulation.
Other tests
Other specific tests are also available with hematological advice. These include specific
- factor assays
- von Willebrand’s factor
- ristocetin-induced platelet aggregation
Tests for other diseases given in the differential diagnosis list should be performed as indicated from the history, examination, and basic laboratory tests.