Table of Contents
Coughing is a nonspecific reaction to irritation anywhere in the respiratory tract from the pharynx to the lungs, and it is the most common manifestation of lower respiratory tract disease. Any cough that persists for over 3 weeks merits further investigation in the absence of an obvious cause.
Differential Diagnosis of Cough and Hemoptysis
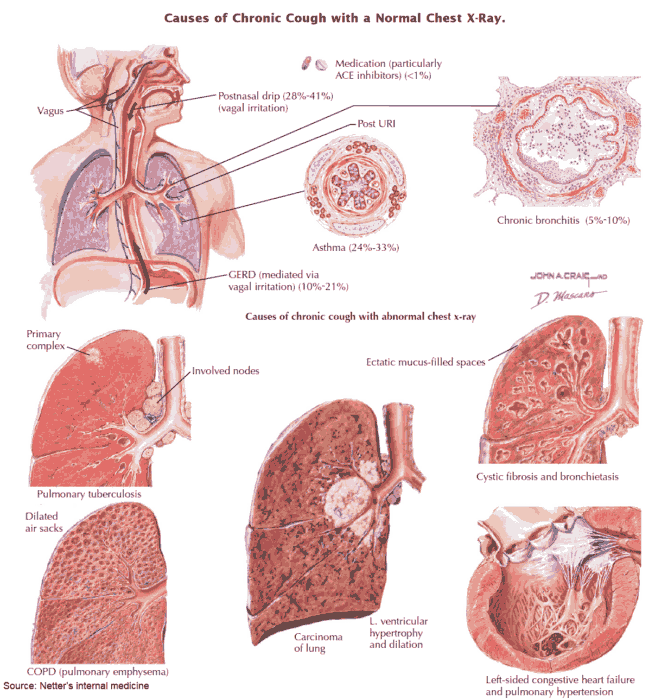
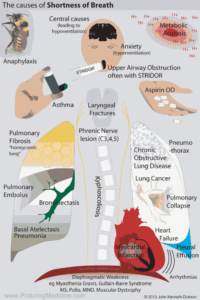
Causes and Differential Diagnosis of Cough
- Postnasal drip: sinusitis.
- Upper respiratory tract infections (e.g., pharyngitis, laryngitis, tracheobronchitis).
- Pressure on the trachea (e.g., from a goiter): this may be associated with stridor.
- Croup and laryngitis.
- Lower respiratory tract causes: almost any lung pathology may be associated with cough, in particular:
- asthma (suspect if there is a nocturnal cough)
- chronic obstructive pulmonary disease (COPD)
- bronchiectasis
- left ventricular failure
- Drugs (e.g., angiotensin-converting enzyme [ACE] inhibitors) and irritants, especially occupational agents.
- Psychogenic cough.
- Nonrespiratory causes (e.g., pericardial irritation, gastroesophageal reflux).
- Causes of hemoptysis.
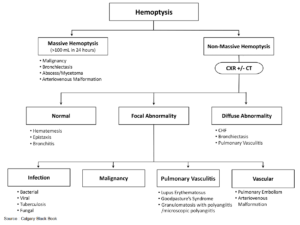
Causes and Differential Diagnosis of Hemoptysis
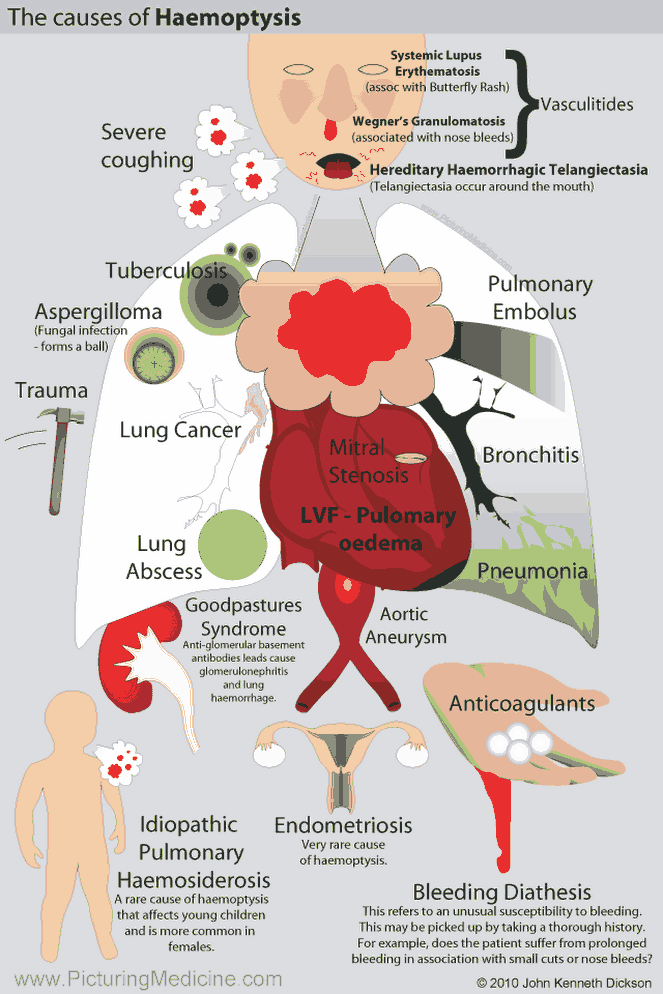
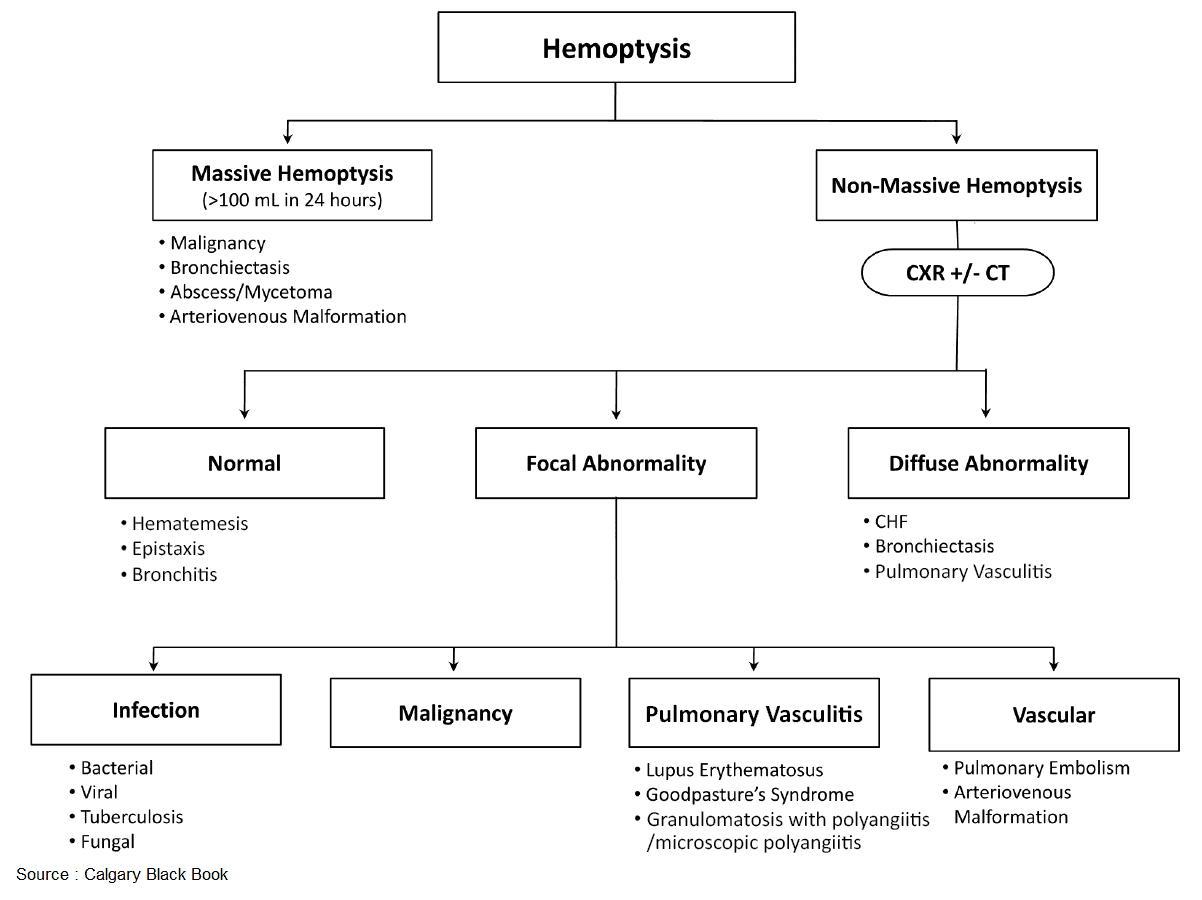
Common causes of hemoptysis include the following:
- Acute infections (e.g., exacerbations of COPD).
- Bronchiectasis: can be responsible for massive hemoptysis.
- Bronchial carcinoma: secondary deposits and benign tumors can also lead to hemoptysis but are less common.
- Pulmonary tuberculosis: a common cause worldwide.
- Pulmonary embolus with infarction.
- Left ventricular failure can lead to the production of pink, frothy sputum.
- Mitral stenosis.
- Other infections, such as lobar pneumonia (“rusty” sputum) or, less commonly, lung abscess.
- Trauma (e.g., contusions to the chest, inhalation of foreign bodies, or after intubation).
Rare causes of hemoptysis include the following:
- Bleeding diatheses.
- Vasculitis (e.g., Goodpasture’s syndrome and Wegener’s granulomatosis).
- Diffuse interstitial fibrosis.
- Idiopathic pulmonary hemosiderosis.
- Arteriovenous malformations (Osler-Weber-Rendu disease [hereditary hemorrhagic telangiectasia], a favorite in exams but rare in practice).
- Eisenmenger’s syndrome.
- Sarcoidosis and amyloidosis.
- Primary pulmonary hypertension.
- Cystic fibrosis.
- Invasive aspergillosis.
Note that in up to 15% of cases no cause for hemoptysis is found.
READ ALSO : Hemoptysis – Causes, Evaluation and Management
History in the Patient with Cough and Hemoptysis
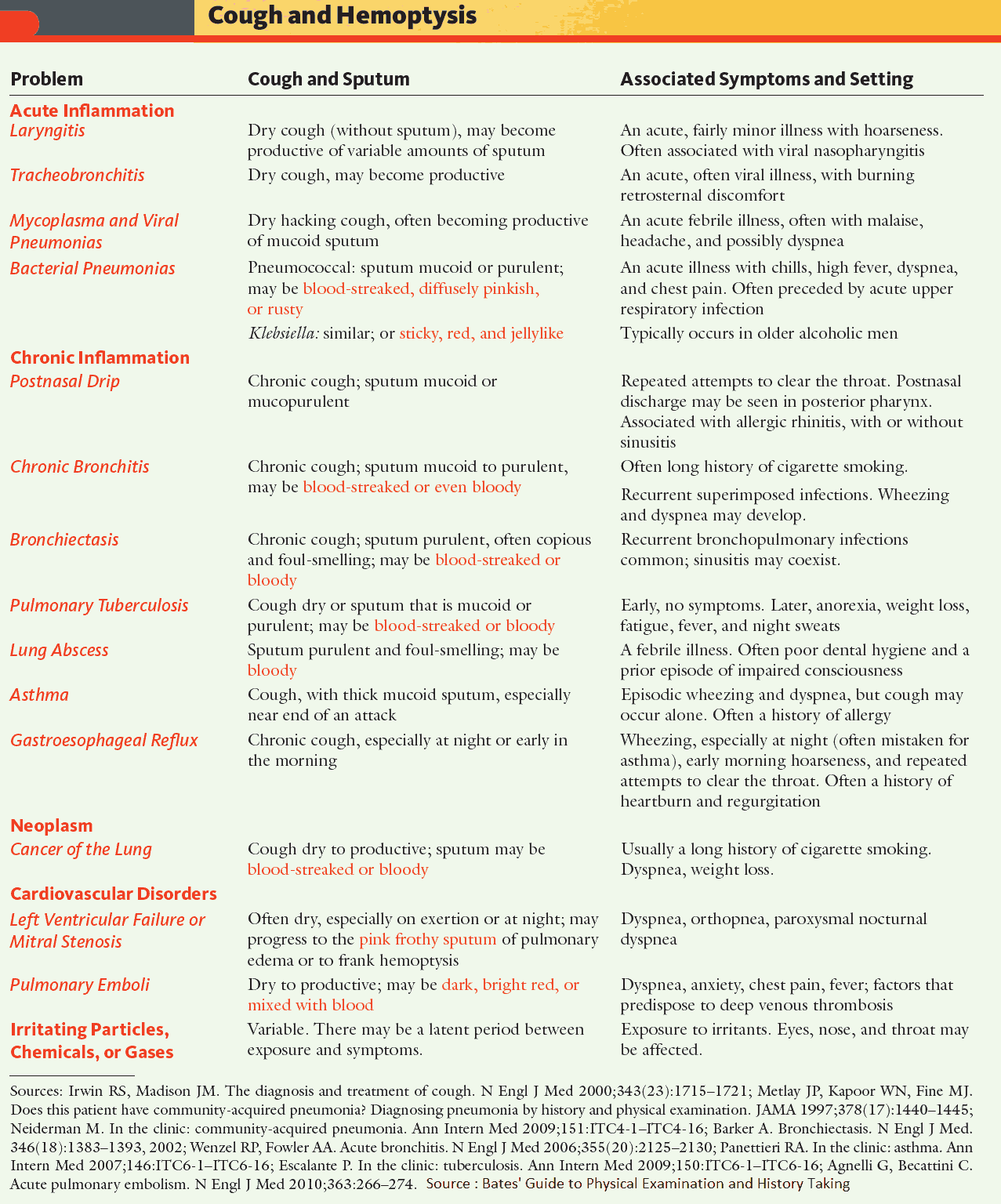
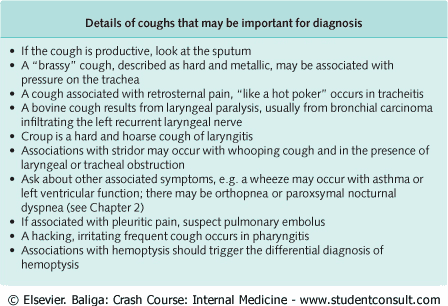
The nature of the cough may help in the diagnosis (image). The following factors should be assessed in the patient with cough or hemoptysis:
- How long has the cough been present? A chronic cough is more commonly associated with tuberculosis, foreign bodies, and asthma.
- Has the patient been in contact with any person with infection or traveled anywhere that has endemic tuberculosis?
- How severe is the cough? Complications include worsening of bronchospasm, vomiting, rib fractures, urinary incontinence, and syncope.
- Does the patient smoke? This can often cause a cough in its own right by acting as an irritant but may also be associated with malignancy.
- Ask about drug history, in particular treatment with ACE inhibitors. Of people on ACE inhibitors, 10-20% will have a dry, tickly cough. It is more common in women than men. The patient may find the cough tolerable once reassured that there is no serious underlying condition, and the ACE inhibitor may be continued if needed. (Note: Angiotensin receptor blockers [ARBs] do not have this side effect.]
- Are there any occupational agents or exposure to dust which might account for the cough?
- Has there been any weight loss? Think of carcinoma or lung abscess. Ask about other features of malignancy if suspected, such as change in bowel habit.
- Has there been a history of trauma to the chest?
- Is there a family history of bleeding disorders?
- Ask about a past history of rheumatic fever-hemoptysis in mitral stenosis.
- If a diagnosis is suspected, ask more leading questions.
- If the patient is a lung transplant recipient or has cystic fibrosis, additional causes need to be considered (acute vs. chronic rejection, cytomegalovirus [CMV] pneumonitis).
- Don’t forget nonrespiratory causes. For example, are there any symptoms suggestive of gastroesophageal reflux disease?
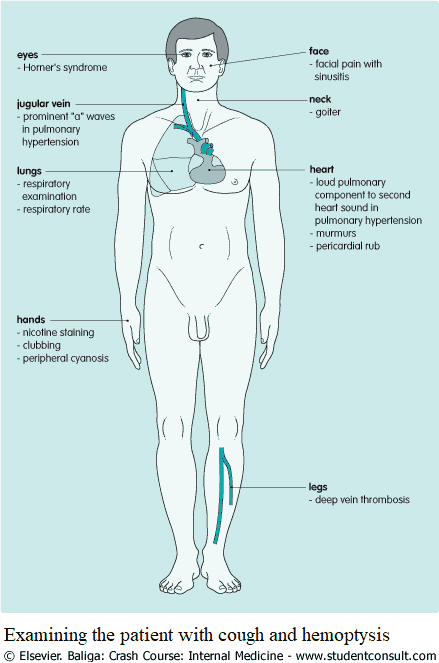
Examining the Patient with Cough and Hemoptysis
Inspection
- If the patient appears breathless, assess the severity and count the respiratory rate.
- Check for anemia: if present think of malignancy, connective tissue diseases, or chronic infection.
- If clubbing is present, suspect bronchial carcinoma, lung abscess, mesothelioma, bronchiectasis, cystic fibrosis, or fibrosing alveolitis.
- If the patient is cyanosed, suspect COPD or Eisenmenger’s syndrome.
- Examine for lymphadenopathy, caused by infections or malignancy.
- Look at the sputum cup if the cough is productive.
- Examine for a goiter. Is there retrosternal extension?
- Examine specifically for signs of bronchial carcinoma (e.g., Horner’s syndrome, paraneoplastic syndromes).
- Examine the legs for DVT, with pulmonary embolus as a cause for hemoptysis.
- Look at the skin. Punctate lesions on mucus membranes are present with Osler-Weber-Rendu disease.
- Check for facial pain in sinusitis.
Auscultation
Proceed to a full respiratory examination, including:
- auscultation for murmurs over the lung fields with arteriovenous malformations
- bronchial breathing in lobar consolidation
- fine crackles with left ventricular failure and fibrosing alveolitis
- coarser crackles in bronchiectasis
- a localized wheeze, not disappearing on coughing, suggests a blocked major airway from a carcinoma or a foreign body.
Examining Other Systems
- Auscultate the heart for the murmur of mitral stenosis or a pericardial rub.
- Listen for the pleural rub of pulmonary infarction.
- In pulmonary hypertension, there will be a loud pulmonary component of the second heart sound, a right ventricular heave, a pulmonary systolic murmur, and prominent a-waves in the jugulovenous pressure. This also may lead to the other physical findings of right ventricle failure, such as peripheral edema and hepatic tenderness.
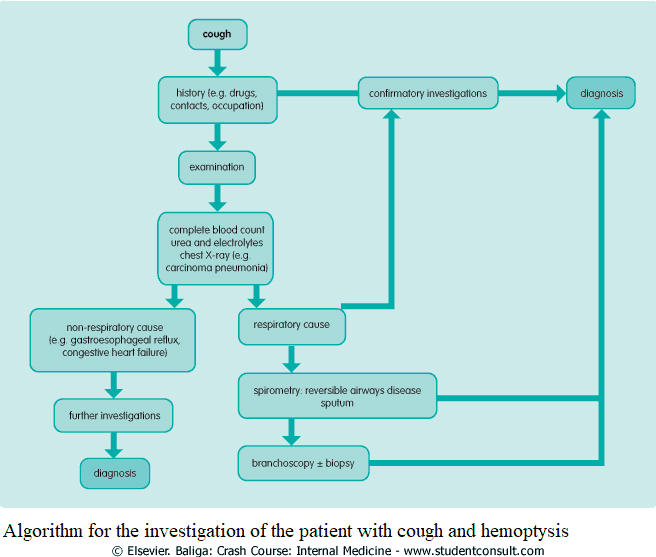
Investigating the Patient with Cough and Hemoptysis
The following investigations should be performed in the patient with cough or hemoptysis:
- Complete blood count: anemia with malignancies, leukocytosis with infection, eosinophils with aspergillosis or allergies.
- Blood cultures: help define infection. Viral titers can be drawn but probably will not influence treatment.
- Basic metabolic panel.
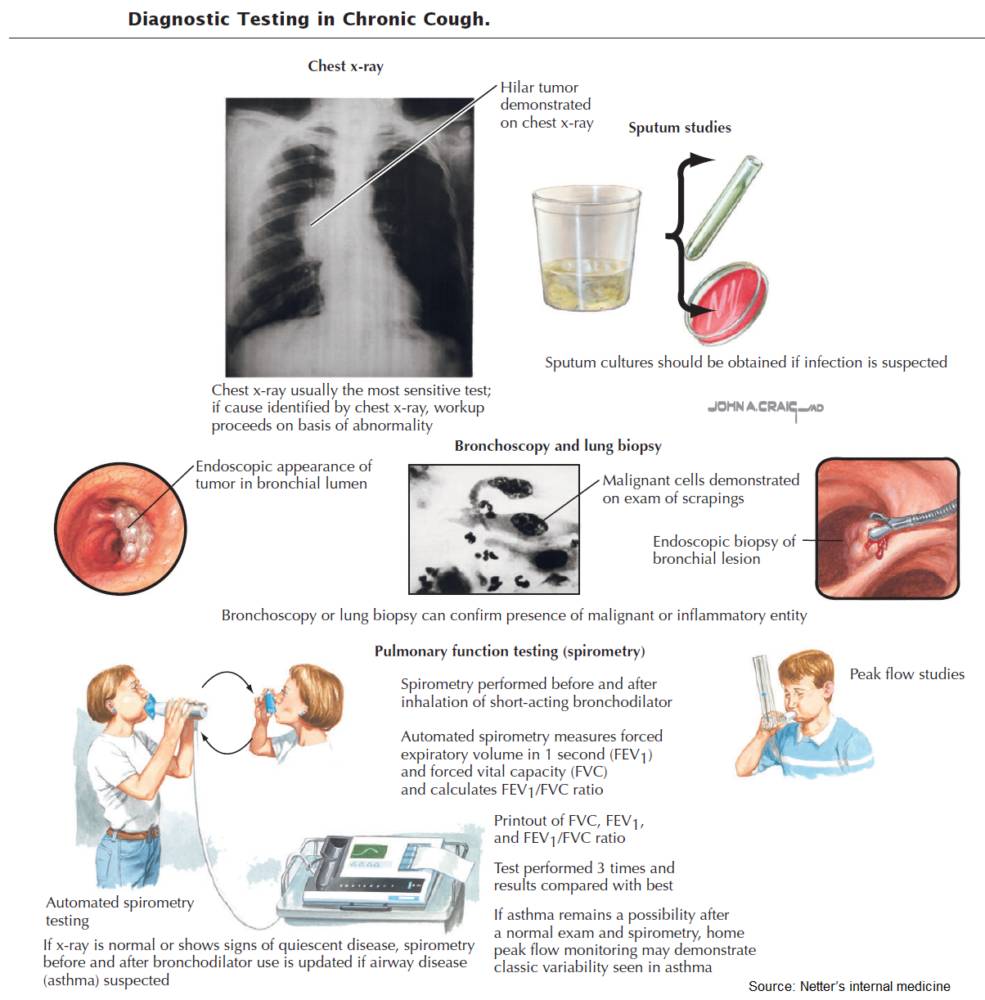
- Chest x-ray: this may reveal the pulmonary cause of the cough (e.g., pneumonia, a straight left heart border with mitral stenosis, infiltrative lung diseases, honeycombing or cyst formation with bronchiectasis, bilateral hilar lymphadenopathy in sarcoidosis).
- Sputum: microscopy, culture, and cytology.
- Pharyngoscopy: if an upper respiratory cause is suspected.
- Ventilation/perfusion scan: if a pulmonary embolus is suspected.
- Bronchoscopy with or without biopsy-if infection is still unknown or if neoplasm/interstitial lung disease is suspected.
- Specific lung function tests: if the cause has not been found after the above tests have been carried out.
- High-resolution computed tomography: to confirm the presence of interstitial disease; it is useful in confirming bronchiectasis.
- Gastroscopy or barium meal: to investigate possible gastroesophageal reflux disease.