Table of Contents
Early Identification of Sepsis
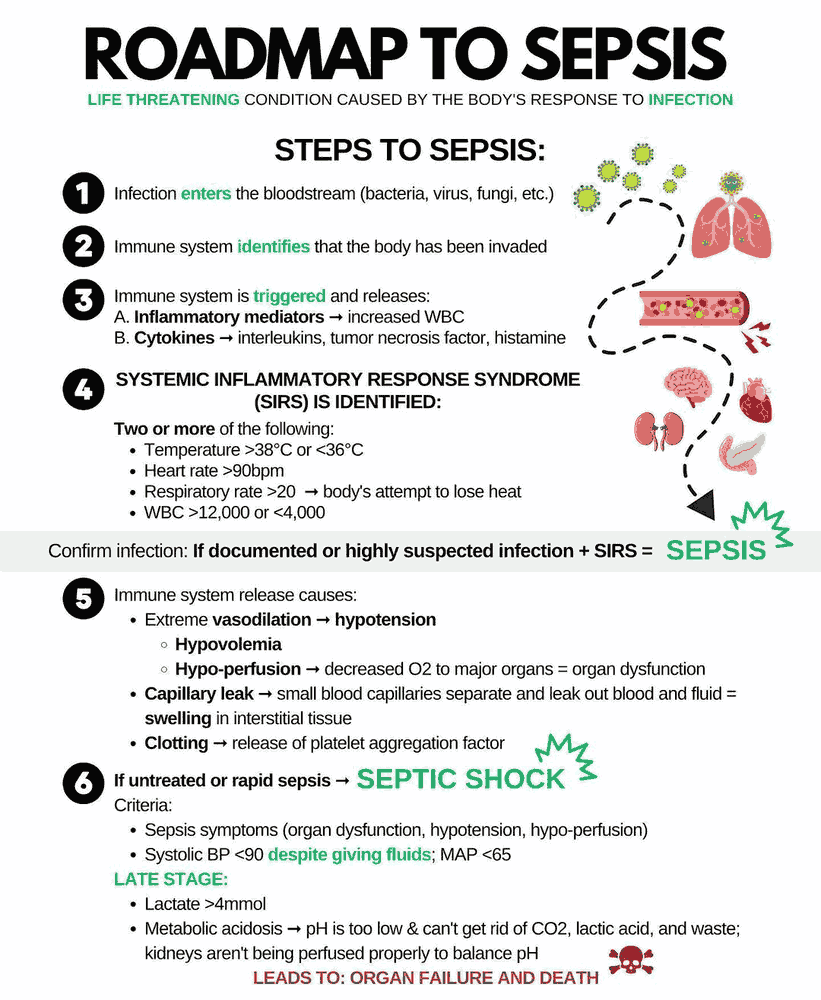
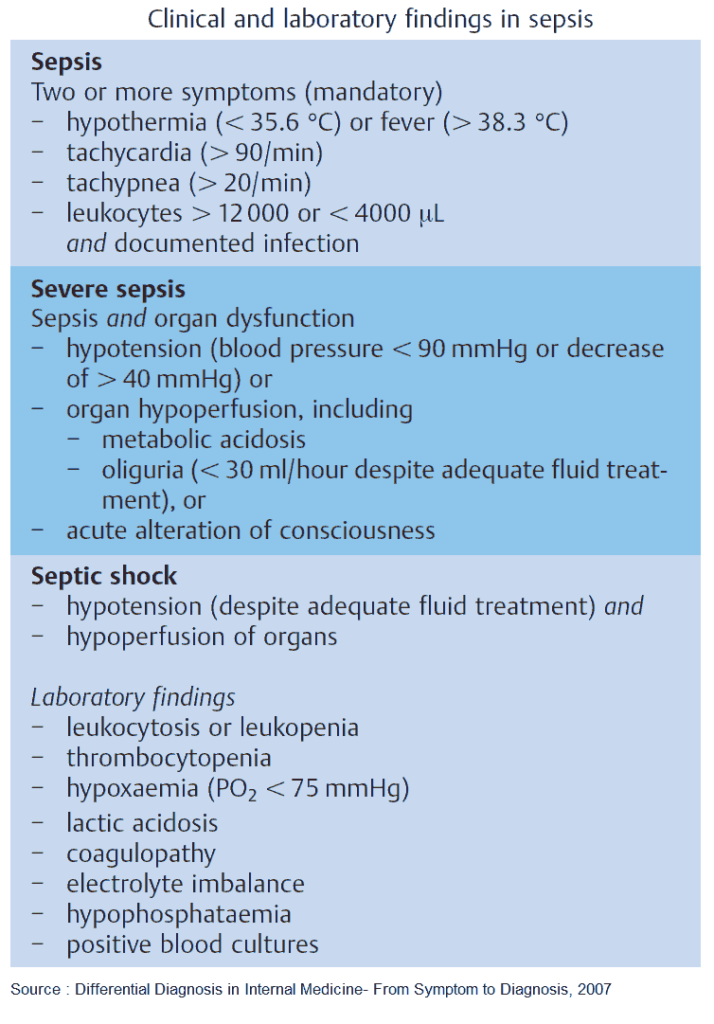
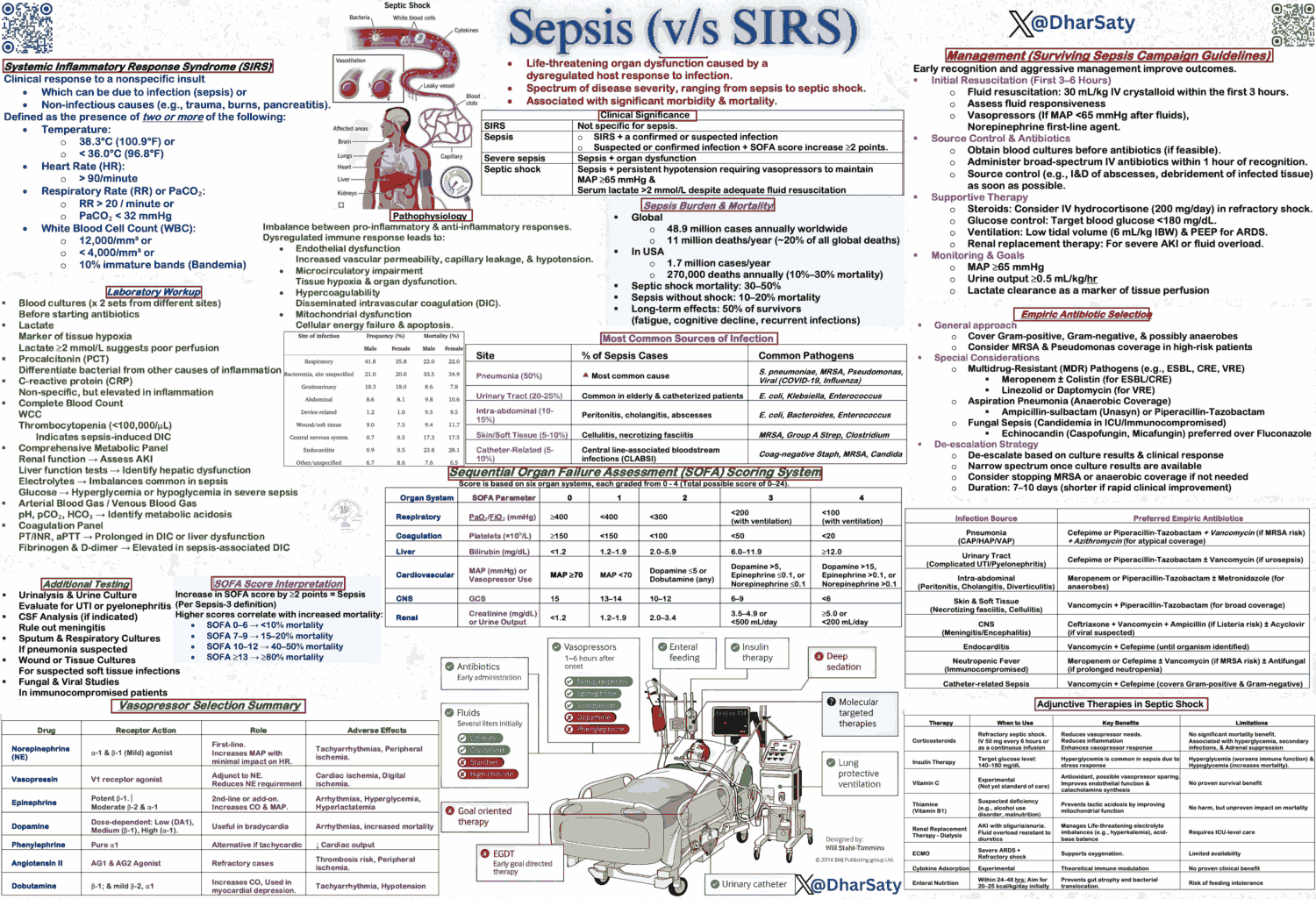
SIRS (Systemic Inflammatory Response Syndrome)
- Inflammatory response to a non-infectious insult (pancreatitis, burn, surgery…)
- Temperature (<36 or >38°C)
- Tachycardia (HR >90)
- Tachypnea (RR > 20 or PaCO2 < 32)
- WBC (>12,000, <4,000 or >10% bands)
Sepsis
- Systemic, deleterious inflammatory response to infection
- Diagnosis: Infection (documented or suspected) and some of the following:
- General variables
- Fever (> 38.3°C)
- Hypothermia (core temperature < 36°C)
- Heart rate > 90
- Tachypnea
- Altered mental status
- Significant edema or positive fluid balance (> 20 mL/kg over 24 hr)
- Hyperglycemia (plasma glucose > 140mg/dL in the absence of diabetes)
- Inflammatory variables
- Leukocytosis (WBC count > 12,000)
- Leukopenia (WBC count < 4000)
- Normal WBC count with greater than 10% immature forms (bands)
- Plasma C-reactive protein more than two standard deviations (sd) above the normal value
- Plasma procalcitonin more than two standard deviations (sd) above the normal value
- Hemodynamic variables
- Arterial hypotension (SBP < 90mm Hg, MAP < 70mm Hg, or an SBP decrease > 40mm Hg in adults or less than two sd below normal for age)
- Organ dysfunction variables
- Arterial hypoxemia (PaO2/FiO2 < 300)
- Acute oliguria (urine output < 0.5 mL/kg/hr for at least 2 hrs despite adequate fluid resuscitation)
- Creatinine increase > 0.5mg/dL
- Coagulation abnormalities (INR > 1.5 or aPTT > 60 s)
- Ileus (absent bowel sounds)
- Thrombocytopenia (platelet count < 100,000)
- Hyperbilirubinemia (plasma total bilirubin > 4mg/dL)
- Tissue perfusion variables
- Hyperlactatemia (High Lactate)
- Decreased capillary refill or mottling
- General variables
Sepsis induced hypotension
- SBP < 90 mm Hg or MAP < 70 mm Hg or
- SBP decrease > 40mm Hg in the absence of other causes of hypotension.
Severe sepsis
- Sepsis + organ dysfunction
- Definition: Sepsis induced tissue hypoperfusion or organ dysfunction with any of the following thought to be due to the infection
- Sepsis-induced hypotension
- Lactate above upper limits of laboratory normal
- Urine output <0.5 mL/kg/hr for more than two hours despite adequate fluid resuscitation
- Acute lung injury with PaO2/FIO2 <250 in the absence of pneumonia as infection source
- Acute lung injury with PaO2/FIO2 <200 in the presence of pneumonia as infection source
- Creatinine >2 mg/dL
- Bilirubin >4 mg/dL
- Platelet count <100,000
- Coagulopathy (INR >1.5)
- Mortality rate: 25-30%
Septic Shock:
- Mortality rate: 40-70%
- Severe sepsis + hypotension, not responsive to fluid resuscitation
- Sepsis induced hypotension persisting despite adequate fluid resuscitation (30ml/kg)
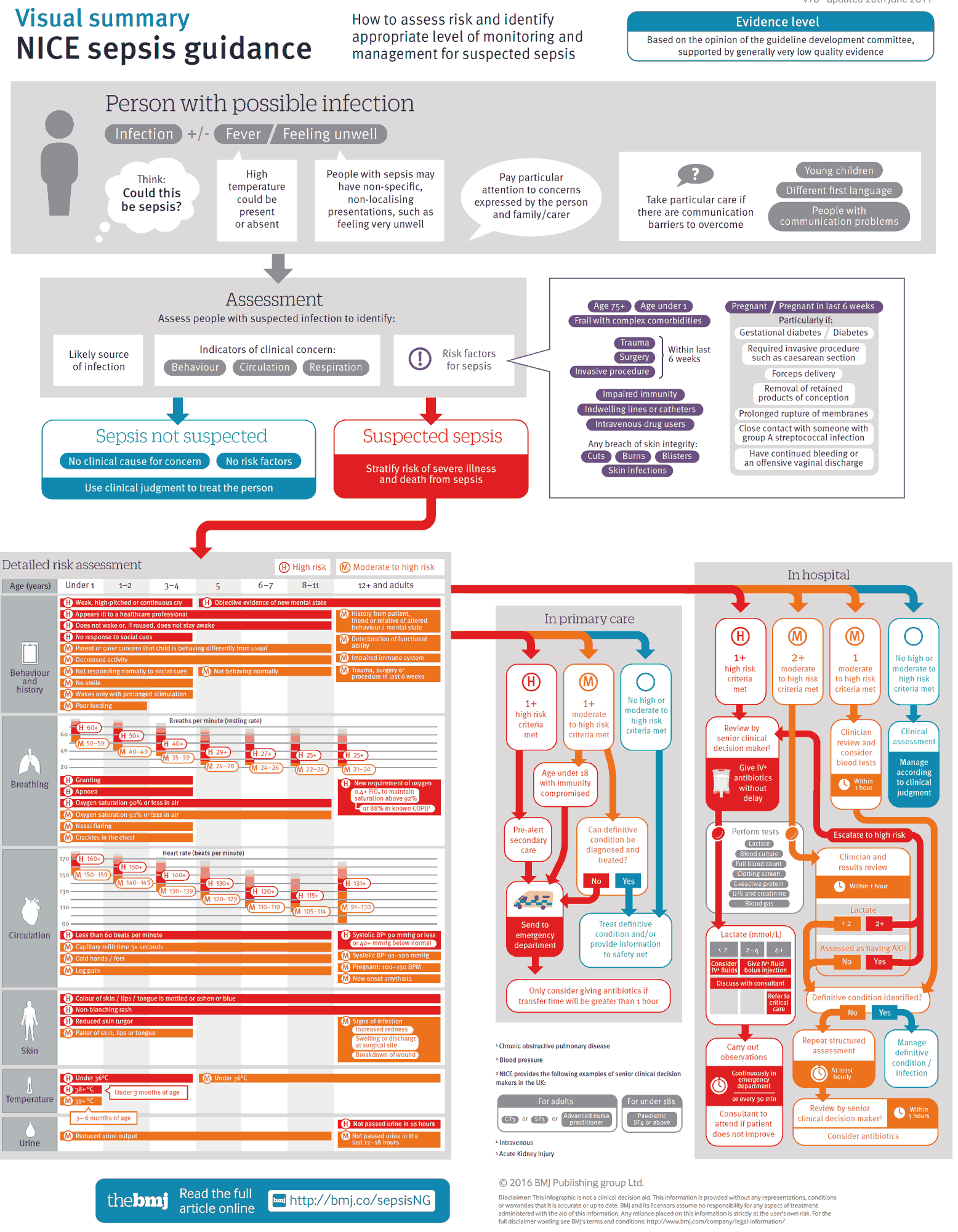
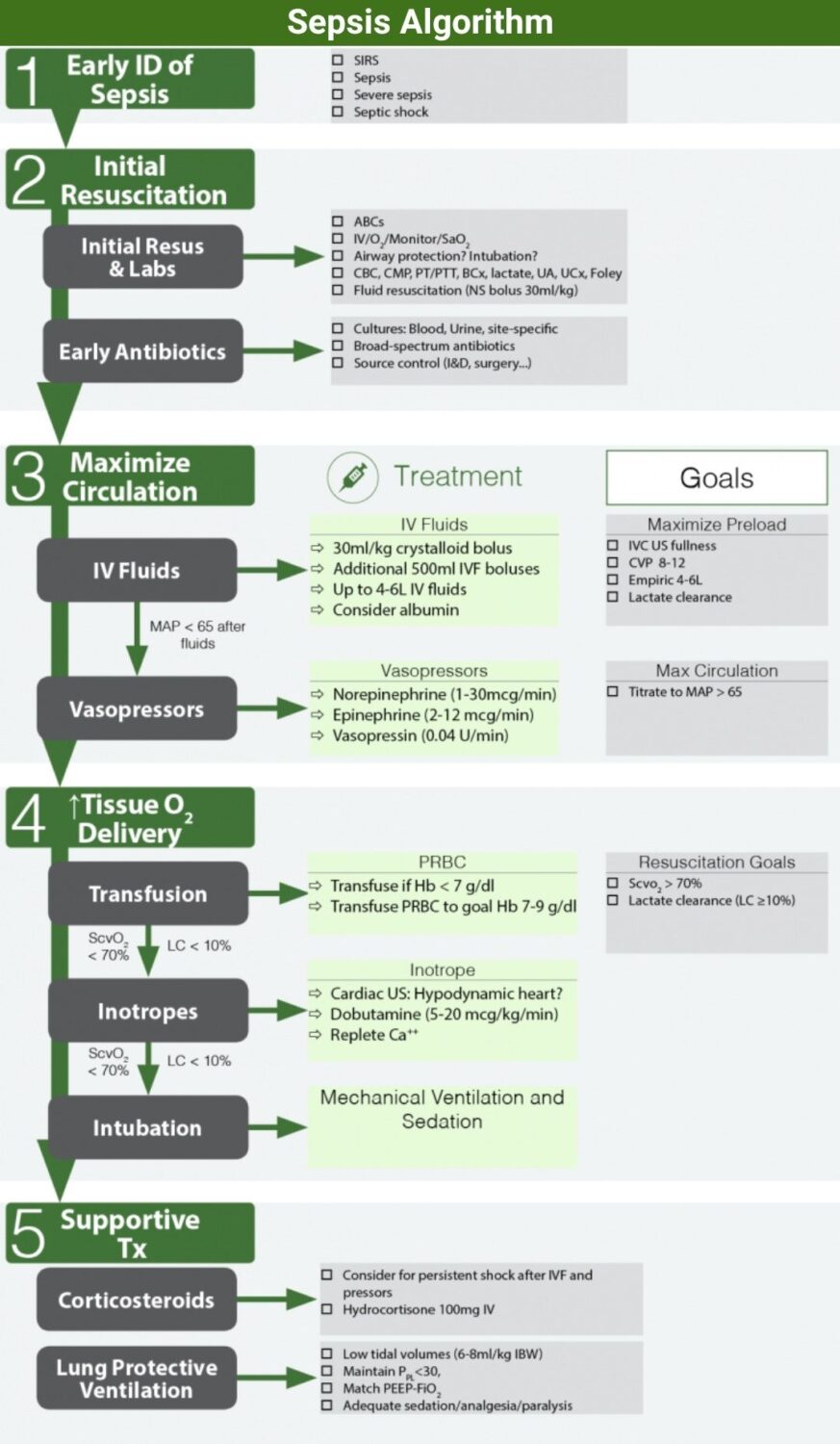
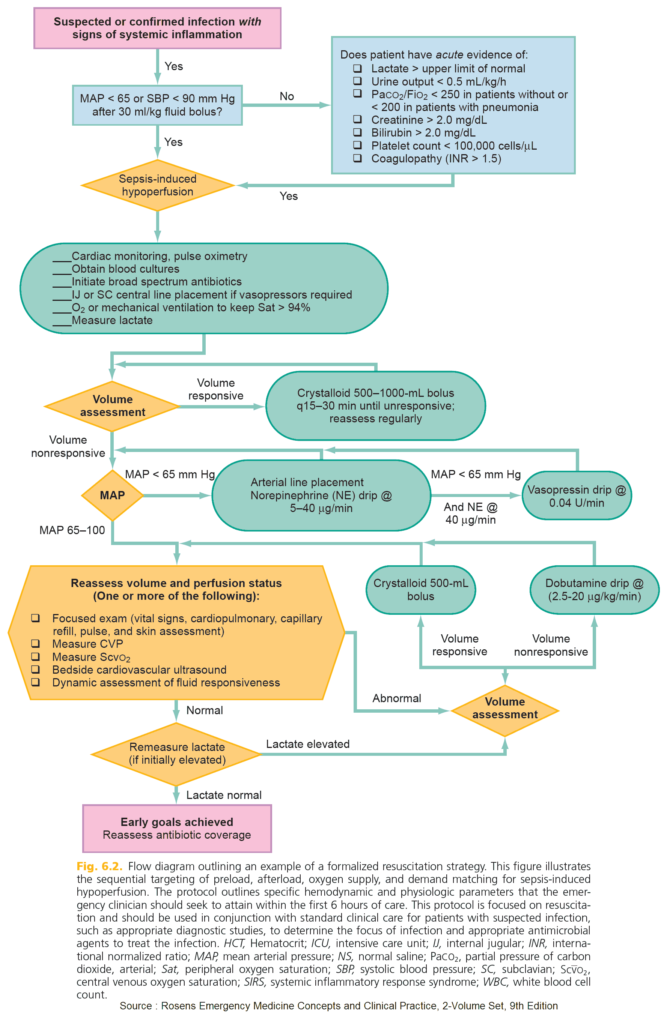
Initial Resusctitation
Initial Resuscitation
- ABCs / IV / O / Monitor / SaO22
- Labs: CBC, CMP, PT/PTT, BCx x 2, lactate, UA, UCx, Foley
- Fluid resuscitation (30ml/kg Normal Saline bolus to start)
- Early broad spectrum antibiotics
- Consider central line +/- CVP monitoring
Oxygenation
- Goal: maximize O2 delivery to tissue
- Supplemental oxygen for all patients
- Consider Intubation?
- Altered mental status and unable to protect airway
- Persistent hypoxia despite (SaO2 < 90%) despite O2 supplementation (non-rebreather mask)
- Severe hypotension/shock
- Respiratory failure
Resuscitation End Goal
Maximize Tissue Oxygen delivery as measured by:
□ ScvO2 > 70%
□ Lactate clearance (LC) ≥10%
Goals
- CVP 8–12 mm Hg
- MAP ≥ 65 mm Hg
- Urine output ≥ 0.5 mL/kg/hr
- Superior vena cava oxygenation saturation (ScvO) 70% or mixed venous oxygen saturation (SvO2) 65%
Target
- Target: Normalizing lactate (in patients with elevated lactate)
Early Antimicrobials
- Blood Cultures
- 2 sets, at least one peripheral and one via each vascular device
- Cultures before antibiotics if no significant delay (>45 min)
- Cultures from other sites (CSF, Urine, body fluids) should also be obtained before antibiotics if no delay
- Antibiotics
- Begin broad-spectrum empiric antibiotics within one hour of diagnosis of sepsis to cover likely source and pathogens
- Each hour delay in antibiotics is associated with a measurable increase in mortality
Antibiotics
□ Blood cultures prior to antibiotics
□ Antibiotics within 1 hour of diagnosis
Source control
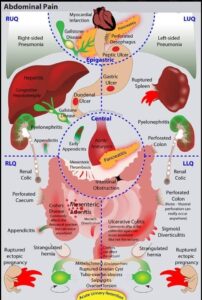
- Evaluate patient for focus of infection amenable to source control (abscess drainage, debridement, device removal etc..)
- Look for cause of infection that can be surgically controlled (peritonitis, cholangitis, intestinal infarction, necrotizing soft tissue infection etc.)
- If intravascular access devices are a possible source, they should be removed promptly after other vascular access has been established
Maximize Circulation
Fluids (Preload)
- Crystalloids
- Initial fluid of choice
- Initial fluid challenge: 30ml/kg (2-3L) bolus
- Additional fluid in boluses (500ml) and reassess after each bolus
- Goal (maximize preload)
- Goal → No additional stroke volume from more fluids
- Empiric IV fluids: Begin with 30ml/kg bolus and continue up to 4-6 L (goal MAP>65)
- IVC US: Fluid bolus until there is ↓ change in size of IVC with respiration
- CVP monitoring: Fluid bolus until goal CVP >10 (CVP>14 in intubated pts)
- ProCESS trial showed no benefit to using invasive monitoring and CVP measurements
- Caution:
- Cardiogenic pulmonary edema
- Non-Cardiogenic pulmonary edema (ARDS) → more fluid worsens prognosis
- Albumin
- Indication: Patient has already received a substantial amount of crystalloid (4-6L) → use albumin to help prevent third spacing
- Dose: 500cc bolus of 5% albumin (or a dose of 25% albumin)
- Journal club
- Meta-analysis (Crit Care Med 2011; 39:386–391)
- Use of albumin solutions for the resuscitation of patients with sepsis was associated with lower mortality compared with other fluid resuscitation regimens.
- SAFE study (N Engl J Med 2004;350:2247)
- Similar outcomes for saline and albumin
- ALBIOS Trial (N Engl J Med 2014; 370:1412)
- No improved survival at 28 and 90 days when with albumin added to crystalloid
- Meta-analysis (Crit Care Med 2011; 39:386–391)
MAP formula
MAP = (2 x DBP + SBP) / 3
Vasopressors
- Indication: MAP <65 after adequate fluid loading
- Goal: Target MAP > 65 mmHg
- Supplemental endpoints: Blood Pressure, regional/global perfusion, urine output, mental status, lactate
- Norepinephrine (Levophed-NE)
- First line drug of choice
- Dose:
- Start: 0.5-1 mcg/min (up to 30mcg/min in refractory shock)
- Increases MAP due to its vasoconstrictive effects, with little change in heart rate and less increase in stroke volume compared with dopamine
- Norepinephrine vs Dopamine (N Engl J Med 2010;362:779)
- No overall difference in mortality (52.5% vs 48.5%; p= 0.10)
- Increased rate of arrhythmias with Dopamine (24.1% vs 12.4%)
- Increased mortality in patients with cardiogenic shock with Dopamine
- Epinephrine
- 2nd line agent to be added to or substituted for Norepinephrine
- Dose: 2-10 mcg/min IV
- Vasopressin
- Dose:
- 0.04 U/min IV
- Can be added to Norepinephrine with the intent of raising MAP to target or decreasing Norepinephrine dosage
- Not recommended as single agent
- Dose:
- Dopamine
- Alternative to Norepinephrine only in highly selective patients
- Dose:
- Low-dose: 1-5 mcg/kg/minute, increased renal blood flow and urine output
- Intermediate-dose: 5-15 mcg/kg/min: ↑ renal blood flow, heart rate, cardiac contractility, and Cardiac Output (CO)
- High-dose: >15 mcg/kg/min alpha-adrenergic effects predominate, vasoconstriction, increased Blood Pressure
- Phenylephrine
- Not recommended except in certain circumstances:
- Patient at risk for arrhythmias (Norepinephrine is associated with serious arrhythmias)
- Cardiac output is known to be high and blood pressure persistently low
- Salvage therapy when combined inotrope/vasopressor drugs and low-dose vasopressin have failed to achieve the MAP target
- No Central line: can be given peripherally temporarily
- Dose:
- 40-60 mcg/min IV (Start 100-180 mcg/min IV until Blood Pressure stable)
- Not recommended except in certain circumstances:
Vasopressors
Ensure that patient is adequately hydrated before starting vasopressors
Maximize Tissue Oxygen Delivery
Resuscitation end points:
- Vital sign endpoints (MAP, BP, HR etc…) are not sufficient to gauge adequacy of resuscitation and tissue hypoxia
- Patients resuscitated to normal VS may continue to have tissue hypoxia as evidenced by decreased lactate clearance and persistently low ScvO (Am J Emerg Med 1996;14(2):218)
- Goals of resuscitation:
- Superior vena cava oxygenation saturation (ScvO2) > 70%
- Lactate clearance (LC) ≥10%
Lactate clearance (LC)
- Goal: lactate clearance by at least 10%
- Lactate as predictor of mortality
- Mortality rates increase as lactate increases (Ann Emerg Med. 2005;45:524)
- As lactate increases from 2 to 8 mg/dL, mortality increases from 1090% (Crit Care Med 1992;20:80)
- Lactate clearance (↓ lactate ≥ 10%)
- Alternative to ScvO2 (JAMA 2010;303:739):
- Lactate clearance may be acceptable alternative to ScvO2 in determining tissue perfusion
- Lactate clearance of at least 10% over ≥ 2 hours (adequate tissue oxygen delivery) produces a similar short-term survival rate as a protocol using ScvO2 monitoring.
- Mortality
- The Shock Society (Shock 2009;32:35-3)
- i. Mortality was 60% for lactate non-clearance versus 19% for lactate clearance
- ii. Lactate non-clearance was an independent predictor of death (OR= 4.9)
- iii. ScvO2 optimization did not reliably exclude lactate non-clearance
- Nguyen et. al (Crit Care Med 2004;32:1637)
- i. Lactate clearance had a significant inverse relationship with mortality
- ii. There was an approximately 11% decrease likelihood of mortality for each 10% increase in lactate clearance
- Each 10% increase in repeat lactate values was associated with a 9.4% increase in the odds of hospital death (Ann Am Thorac Soc 2013;10:466)
- The Shock Society (Shock 2009;32:35-3)
- Alternative to ScvO2 (JAMA 2010;303:739):
Lactate Clearance (LC)
Lactate clearance can be used in place of ScvO2 to measure adequacy of resuscitation
IV fluids
- Patient may require additional IV fluids (NS bolus)
- Reassess using CVP (central venous pressure) or Ultrasound as applicable
Inotropic Support
- Dobutamine
- Bedside ECHO/US: Hypodynamic heart?
- Trial of dobutamine for:
- Persistent hypoperfusion (with normal MAP and adequate intravascular volume)
- Myocardial dysfunction
- Dose: up 5-20 mcg/kg/min
- Calcium: replete Ca if low
Blood Products
- Indication: Red blood cell transfusion if hemoglobin concentration decreases to < 7.0 g/dL
- Target a hemoglobin concentration of 7.0 to 9.0 g/dL
- Increases O2 delivery to tissues
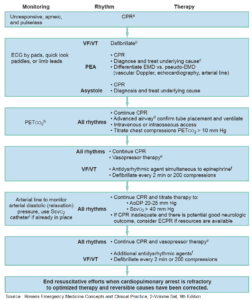
Mechanical Ventilation/Intubation
- Decrease work of breathing and pulmonary metabolic load
Supportive Therapy
- Indication:
- Unable to restore hemodynamic stability with IV fluid resuscitation and vasopressors
- Dose: Hydrocortisone 100mg q8h (200-300mg/d)
- Evidence
- ACTH Stimulation test (not recommended)
- Low cortisol → cortisol levels < 15mcg/dl
- “Non-responder” or “inadequate adrenal reserve” → cortisol levels rise less than 9 mcg/dl to corticotropin stimulation test (250 mcg ACTH stimulation test)
- Option: Check cortisol level before test and 30, 60 min after test
- French trial (JAMA 2002;288:862-871)
- All patient mortality decreased with hydrocortisone (61% vs 55%)
- Mortality benefit was in “non-responders” in septic shock (63% vs 53%)
- No mortality benefit in “responders”
- Conclusion: Survival benefit is seen in patients with adrenal suppression and are non-responders to ACTH stimulation test
- Meta-analysis (BMJ 2004;329:480)
- Overall, randomized controlled trials show that short-course, high-dose steroids do not improve survival in severe sepsis
- Low dose (HCT < 300mg/d) and longer duration of treatment (≥5days) improves hemodynamics, reduces time on vasopressor, and reduces 28 day mortality
- CORTICUS trial (NEJM 2008;358:111-24)
- Hydrocortisone showed no mortality benefit for patients in septic shock, even for patients with “inadequate adrenal reserve”
- Hydrocortisone group → shock was reversed more quickly than in the placebo group (2-3 days)
- Hydrocortisone group
- ACTH Stimulation test (not recommended)
Lung protective ventilation (NEJM 2000;342:1301-1308)
- Avoid high tidal volumes and high plateau pressures in ALI/ARDS
- ARDS-Net protocol:
- 9% decrease in all-cause mortality in patients with Vt 6-8ml/kg (vs 12ml/kg) while aiming for a plateau pressure of <30 cm H2O
- Assist-control Mode ventilation
- Match PEEP to FiO2 requirements
- Maintain SaO2 88-95%
- Permissive hypercapnea (allowing PCO2 to increase above normal) can be tolerated to minimize Vt and PPL
Glucose Control
- Protocolized approach if glucose > 180mg/dl to target upper glucose of < 180 mg/dl
- NICE-SUGAR Trial (N Engl J Med 2009;360:1283)
- Conventional glucose control (<180 mg/dl) resulted in lower mortality vs Intensive glucose control (81108 mg/dl) (Mortality 27.5% vs 24.9%; p=0.02)
- Intensive glucose control protocol also resulted in more episodes of hypoglycemia
- Oral feedings as tolerated
- Bicarbonate not recommended for pH > 7.15
- No evidence supports the use of bicarbonate therapy in the treatment of hypoperfusion induced lactic acidemia associated with sepsis
Other Modalities
- DVT prophylaxis
- Stress ulcer prophylaxis
- Sedation/analgesia/paralysis
- DIC treatment
- Nutrition
Protocols
Early Goal Directed Therapy
- General
- Goal oriented manipulation of cardiac preload, afterload and contractility to achieve a balance between oxygen delivery and oxygen demand
- Resuscitation to EGDT goals in first six hours decreased in-hospital mortality and mortality at 28 and 60 days
- Equipment: Central venous catheter capable of measuring central venous oxygen saturation (ScvO2 and A-Line)
- Maximize Circulation (MAP>65)
- Fluid bolus (NS)
- Goal CVP 8-12 (12-15 for mechanical ventilation) or urine output >0.5ml/kg/hr
- 500-mL bolus of crystalloid every 30 minutes to achieve a CVP of 8-12 mm Hg
- Vasopressors (NEJM 2010;362:779-789)
- Indication: fluid challenge fails to restore blood pressure and adequate perfusion (MAP<65)
- Goal: Vasopressors or vasodilators to achieve MAP 65 mm Hg or SBP 90 mm Hg
- Recommendation: Norepinephrine (first line agent) or Dopamine
- Epinephrine should be used as second line agent in conjunction with Norepinephrine if still need BP support
- Vasopressin can be used as a low-dose background agent (0.04 Units/min) in conjunction with a vasopressor.
- Inotropic therapy (Dobutamine) if adequate MAP/fluid resuscitation but ongoing hypoperfusion
- Fluid bolus (NS)
- Maximize Oxygenation (Goal ScvO2>70%)
- PRBC Transfusion to Hct>30%
- Inotropic agent (Dobutamine) to maximum dose of 20 mcg/kg/min
- Mechanical ventilation & Sedation
ProCESS (N Engl J Med 2014; 370:1683)
- Study protocol
- RCT compared 3 arms of trial:
- EGDT targets (ScvO2, CVP, MAP, UOP;; central access required) vs
- A protocol that used some of the EGDT targets (MAP, UOP; protocol-based standard therapy; central access not required) vs
- Usual care (no protocol used to direct fluid management)
- RCT compared 3 arms of trial:
- Results
- No mortality difference in the three groups (21 versus 18 versus 19 percent)
- No significant benefit of the mandated use of central venous catheterization and central hemodynamic monitoring in all patients