Table of Contents
Resuscitation and Critical Diagnosis
General
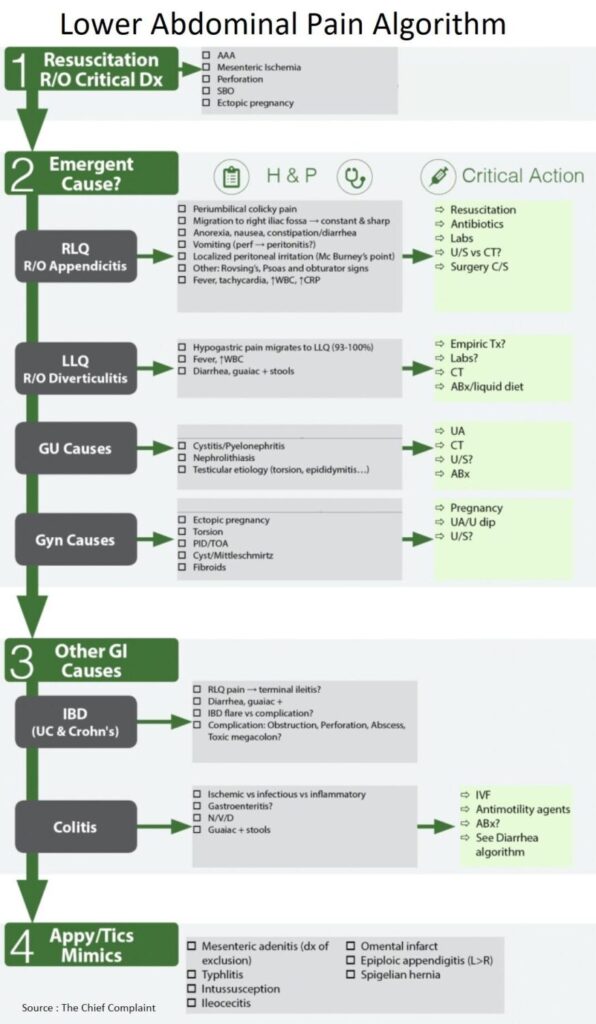
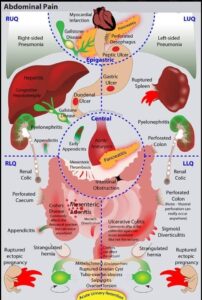
- Work-up for lower abdominal pain begins with resuscitation and exclusion of critical diagnoses
- AAA (Abdominal Aortic Aneurysm)
- Mesenteric Ischemia
- Perforation
- SBO (small bowel obstruction)
- ectopic pregnancy
- Then, through a detailed history and physical, consider all the causes of lower abdominal pain
- Rule out Genitourinary causes (pyelonephritis vs kidney stone) if possible with Urine Analysis
- The differential may then come down to GI (appendicitis, diverticulitis) vs pelvic etiology (in females) → will need further imaging based on suspicion (CT A/P vs pelvic ultrasound)
Resuscitate
• IV/O2/Monitor, IV Fluids, Labs as needed, pregnancy test
Rule Out Critical diagnoses:
• AAA, Mesenteric Ischemia, Perforation, SBO, ectopic pregnancy
Emergent Causes of Lower Abdominal Pain
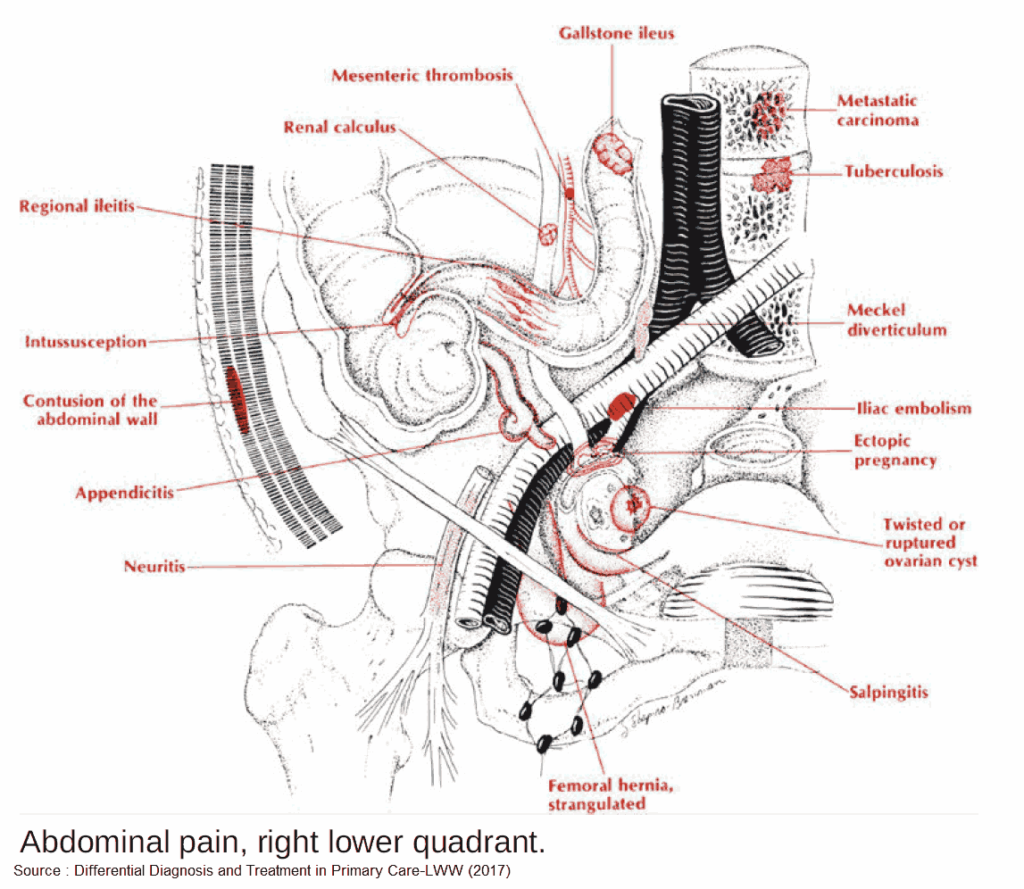
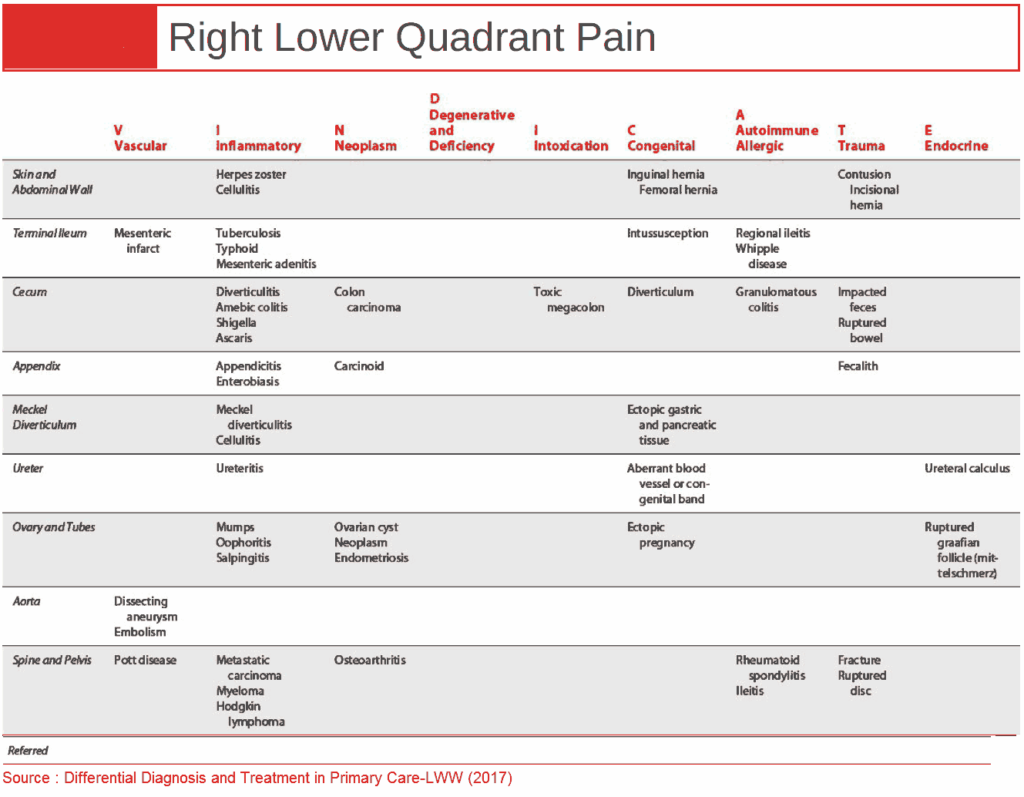
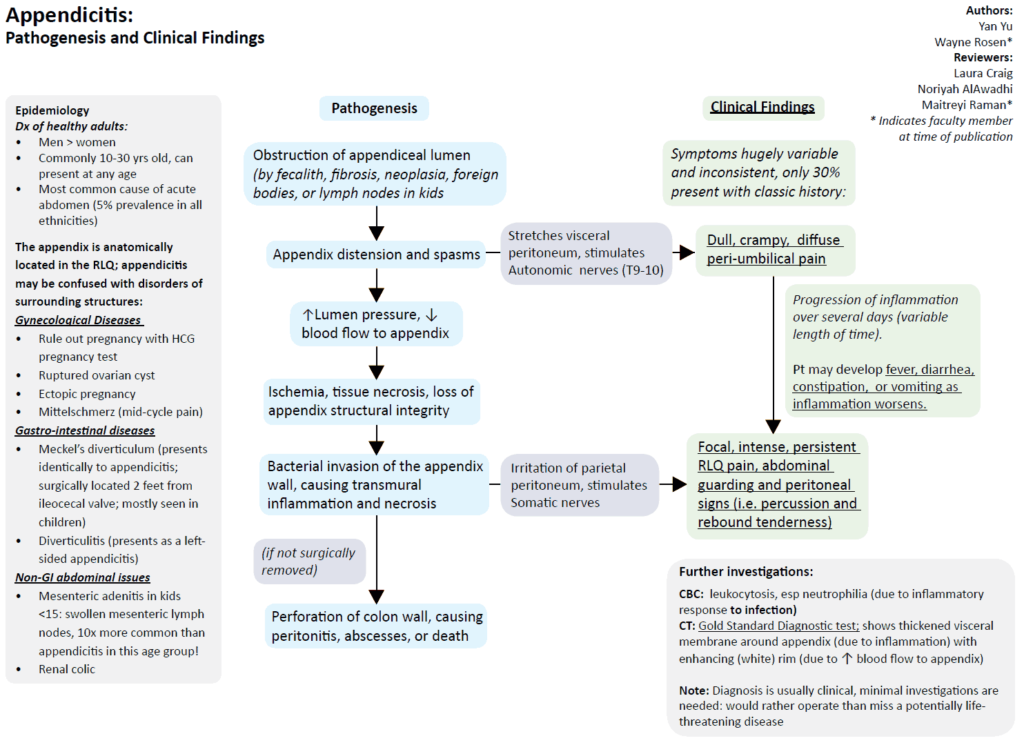
1. Appendicitis
Clinical Presentation of Appendicitis
- General
- Abdominal pain
- Periumbilical colicky pain
- Migration to right iliac fossa → constant and sharp
- Localized peritoneal irritation (McBurney’s point)
- Rovsing’s (palpation in LLQ elicits pain in RLQ)
- Psoas (passive extension of thigh or active flexion of hip → pain → retrocecal appendicitis)
- Obturator signs (flexion and internal rotation of hip → pain)
- Anorexia, nausea / vomiting, constipation / diarrhea
- Fever, tachycardia, High WBC, High CRP
- Abdominal pain
- Strongest predictors of appendicitis (Meta-analysis Brit J Surg 2004;91:28-37)
- Inflammatory response variables (PMN, WBC, CRP)
- Peritoneal irritation (rebound, percussion tenderness, guarding, rigidity)
- Migration of pain (epigastric/periumbilical → RLQ (right lower quadrant))
- Patients at extremes of age may have non-specific symptoms → diagnostic difficulty
Appendicitis Triad
□ Inflammatory markers
□ Peritoneal irritation
□ Migration of pain
Work-up for Appendicitis (Ann Intern Med 2004;141:537-46)
- Ultrasound
- Aperistaltic and non-compressible structure > 6mm
- Sensitivity 86%; Specificity 81%
- CT
- Abnormal appendix, calcified appendicolith + periappendiceal inflammation or diameter >6mm
- Sensitivity 94%; Specificity 95%
Treatment of Appendicitis
- Resuscitation
- Large bore IV, IV Fluids
- Pain control
- Opiate administration has no significant association with management errors (JAMA 2006;296:1764-1774)
- Antibiotics
- Broad spectrum, empiric
- Lower Incidence of postoperative wound infection and intra-abdominal abscess formation (Cochrane Database Syst Rev 2005;(3):CD001439)
- Antibiotics alone for treatment? (Lancet. 2011:377(9777):1573)
- Spontaneous resolution can also occur
- 1 year recurrence rate with antibiotics as sole therapy → 15% most within 10 days
- Surgery
- Risk of rupture: 0-36h → <2%;
- Each ensuing 12h period after 36h → 5%
- Timing (Arch Surg 2006;141:504-7)
- No significant difference between early (<12h after presentation) and later (12- 24h) appendectomy
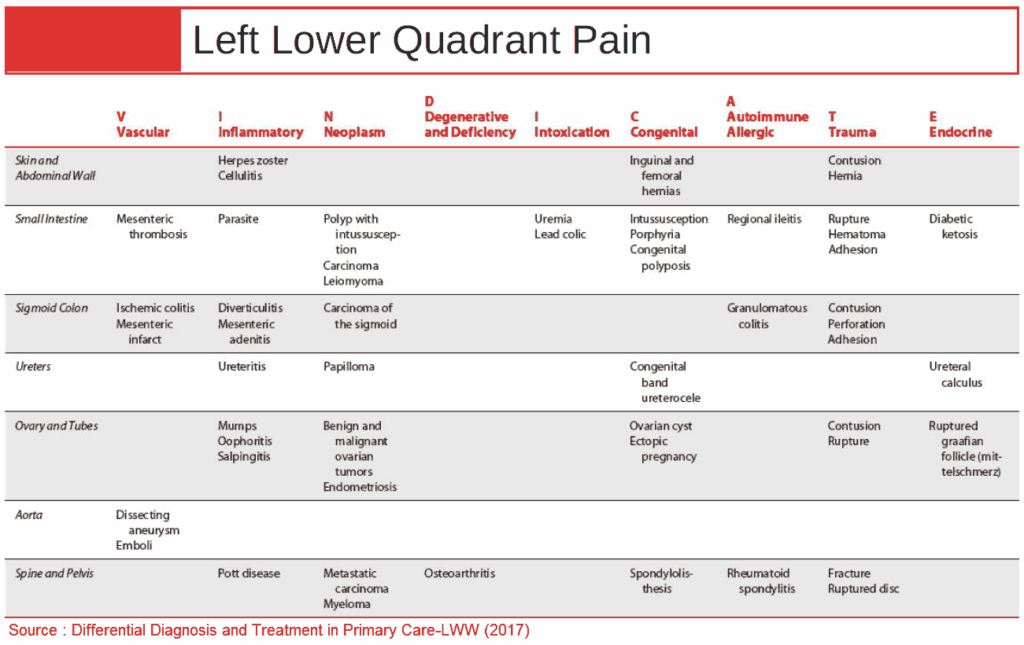
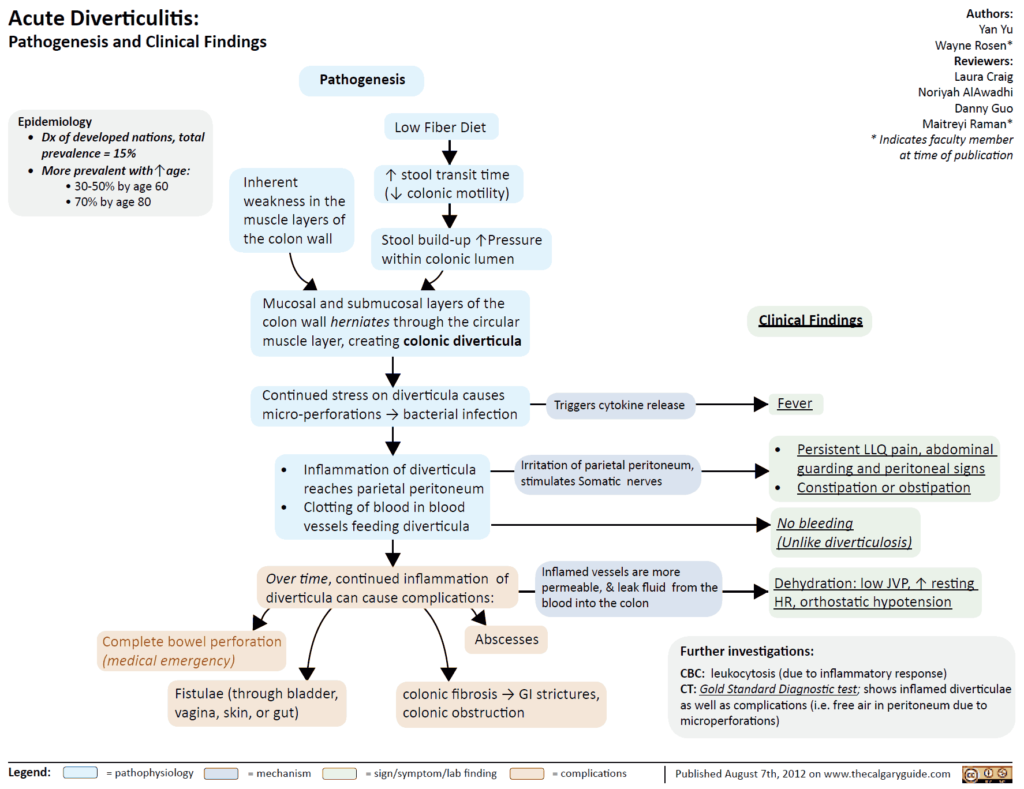
2. Diverticulitis
Clinical Presentation
- Presents like appendicitis, but of the LLQ (lower left quadrant)
- Hypogastric pain migrates to LLQ (93-100%)
- Fever, High WBC
- Diarrhea, guaiac + stools
Work-up for Diverticulitis (Am J Roentgenol 2002;178:1313-8)
- Empiric treatment ?
- No imaging studies needed if diagnosis is clear-cut → can begin empiric treatment
- CT
- Sensitivity 69-95%, Specificity 75-100%
- Use for uncertain diagnosis, exclude other causes of abdominal pain, rule out diverticular complications, or clinical deterioration
- Findings: bowel wall thickening (96%), fat stranding (95%), detects complications (free air, abscess, phlegmons, cancer)
- Ultrasound
- Sensitivity 84%, Specificity 93%
- Rule out AAA, hypoechoic bowel wall thickening, diverticula, abscess, hypoechoic around bowel wall
Complications of Diverticulitis (Emerg Med Clin N Am 2003;21:937-969)
- Abscess
- Can lead to fistula formation, sepsis
- Free perforation, peritonitis
- Rupture of diverticular abscess → acute surgical abdomen
- More common In elderly and immunosuppressed, high mortality (6-25%)
- Fistula
- Fistula between colon and surrounding structures → colovesicular, colovaginal, colocutaneous, coloenteric
- Colovesicular most common (dysuria, pyuria, pneumaturia, fecaluria)
- Obstruction
- Uncommon-2% of cases
- May cause Small-Bowel Obstruction when loops of bowel entangled in peridiverticular adhesions
Treatment of Diverticulitis
- Outpatient
- Indication: Mild symptoms, tolerating oral fluids, well appearing (Am Fam Physician 2005;72(7):1229)
- Antibiotics, 7-10days (Amoxicillin / Clavulanic acid, TMP/SMX (Trimethoprim / Sulfamethoxazole), ciprofloxacin/metronidazole)
- Liquid diet, may consider no antibiotics in extremely well appearing pts (Br J Surg 2012;99(4):532)
- If no improvement in 2-3 days → consider peridiverticular disease (reassessment and admission?)
- Inpatient
- Indication: Severe symptoms requiring narcotics, unable to tolerate oral fluids, elderly, comorbid illnesses, ill/septic, no home support or follow-up
- IV antibiotics (gram negative/anaerobes), bowel rest
- Laparotomy? → generalized peritonitis, sepsis, visceral perforation, clinical deterioration
3. Pyelonephritis
4. Nephrolithiasis
5. Torsion / PID / TOA
6. Acute Scrotum
Other Causes of Lower Abdominal Pain
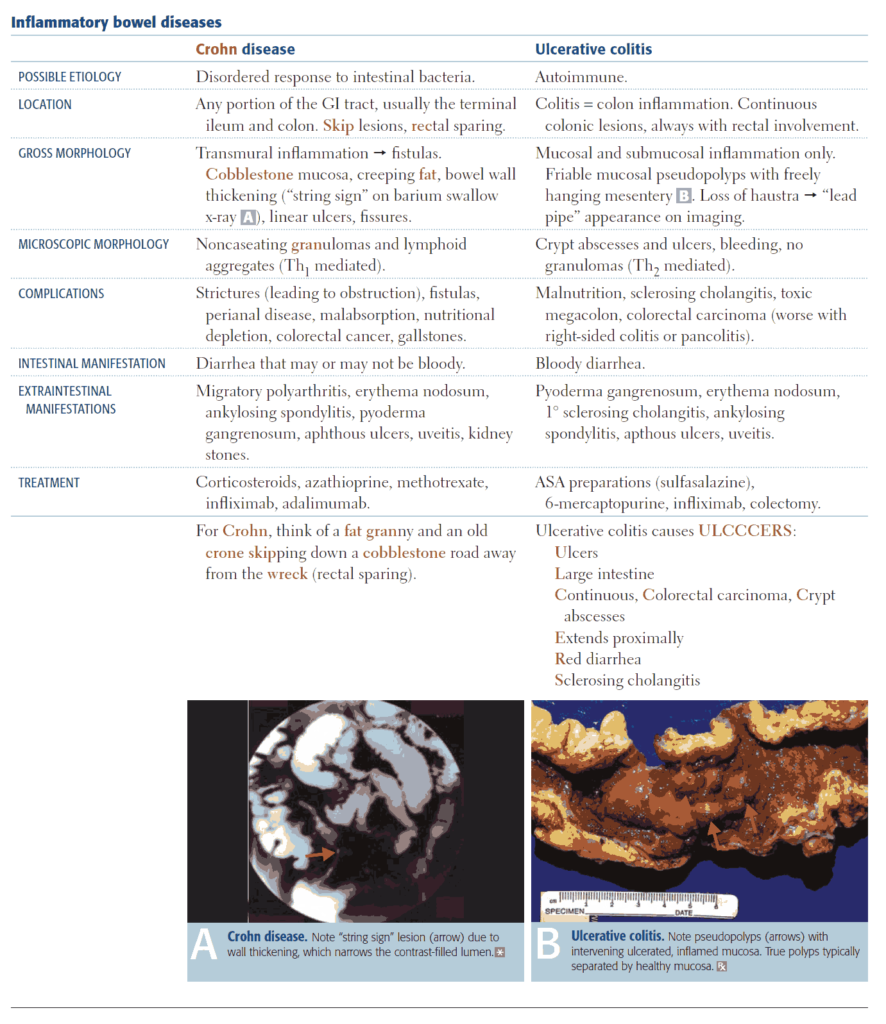
1. IBD (Inflammatory bowel disease)
Clinical Presentation
- RLQ pain → terminal ileitis ?
- Diffuse abdominal pain, diarrhea, guaiac +
Complications
- May be difficult to distinguish “flare” from an acute complication → consider further diagnostic imaging
- TOXIC MEGACOLON
- Define: Lethal complication of IBD or infectious colitis → total or segmental nonobstructive colonic dilatation plus systemic toxicity
- Clinical: abrupt onset bloody diarrhea, fever, High WBC, tachycardia, third space losses, ill appearing, abdominal distension → perforation (peritoneal signs may be masked by steroids)
- Therapy: Resuscitation, blood transfusion, broad spectrum antibiotics, corticosteroids, +/- immunosuppressants, bowel rest and bowel decompression
- Surgery: indicated if no improvement on medical therapy (subtotal colectomy with endileostomy)
- Hemorrhage: (CD > UC) → Resuscitation, blood transfusion, surgery consult (bowel resection?)
- Other: Obstruction, Perforation, Abscess
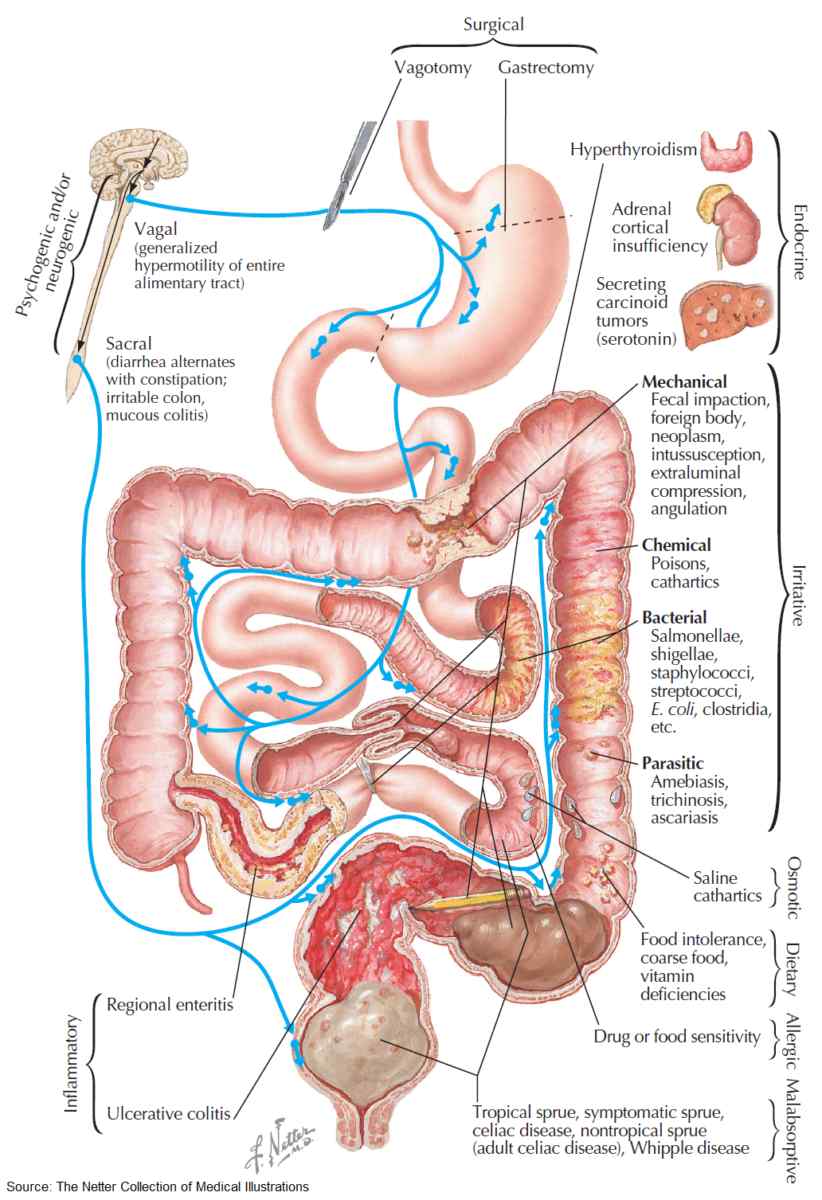
2. Colitis
- Etiology
- Ischemic vs infectious vs inflammatory
- Mesenteric Ischemia
- Clinical Presentation
- Gastroenteritis ?
- N/V/D
- Guaiac + stools
Other Appendicitis Mimics
- Mesenteric adenitis (diagnosis of exclusion)
- Typhlitis
- Intussusception
- Ileocecitis
- Omental infarct
- Epiploic appendigitis (L>R)
- Spigelian hernia
References
- https://www.bmj.com/content/333/7567/530
- https://pubmed.ncbi.nlm.nih.gov/20116016/
- https://pubmed.ncbi.nlm.nih.gov/14716790/
- https://pubmed.ncbi.nlm.nih.gov/15466771/
- https://jamanetwork.com/journals/jama/article-abstract/203613
- https://pubmed.ncbi.nlm.nih.gov/16034862/
- https://pubmed.ncbi.nlm.nih.gov/21550483/
- https://jamanetwork.com/journals/jamasurgery/article-abstract/398369
- https://pubmed.ncbi.nlm.nih.gov/12034590/
- https://pubmed.ncbi.nlm.nih.gov/14708814/
- https://pubmed.ncbi.nlm.nih.gov/16225025/
- https://pubmed.ncbi.nlm.nih.gov/22396052/